Vol 8 No 2 2023 – 10

Prognostic index of hypertensive cardiopathy evolutionary changes: from mild diastolic dysfunction to depressed systolic function.

Alexis Álvarez-Aliaga1* , Liannys Lidia Naranjo Flores1
, Liannys Lidia Naranjo Flores1 , Alexis Suárez-Quesada1
, Alexis Suárez-Quesada1 , David Salvador del Llano-Sosa1
, David Salvador del Llano-Sosa1 , Andrés José Quesada Vázquez1
, Andrés José Quesada Vázquez1 , Adonis Frómeta Guerra1
, Adonis Frómeta Guerra1 .
.
 , Liannys Lidia Naranjo Flores1
, Liannys Lidia Naranjo Flores1 , Alexis Suárez-Quesada1
, Alexis Suárez-Quesada1 , David Salvador del Llano-Sosa1
, David Salvador del Llano-Sosa1 , Andrés José Quesada Vázquez1
, Andrés José Quesada Vázquez1 , Adonis Frómeta Guerra1
, Adonis Frómeta Guerra1 .
.1 Carlos Manuel de Céspedes General University Hospital of Bayamo, Granma Province, Cuba
Correspondong author. alexis.grm@infomed.sld.cu
Available from: http://dx.doi.org/10.21931/RB/2023.08.02.10
ABSTRACT
Hypertensive cardiopathy is a variable and complex group of effects that can provoke a chronic elevation of arterial pressure in the heart. Its morbidity and mortality are increasing. To evaluate the capacity of an index based on prognostic factors to predict the evolution of hypertensive cardiopathy with mild diastolic dysfunction to depressed systolic function. We carried out a prospective cohort study in patients with hypertensive cardiopathy, followed at the specialized arterial hypertension physician’s office of the Specialty Policlinic attached to «Carlos Manuel de Céspedes» General University Hospital, Bayamo Municipality, Granma Province, Cuba. The period evaluated was from Jan 1, 2008, to Dec 31, 2021. The patients followed had at least four appointments per year. Index internal validity. The mean values of the proposed index were twice as high in patients with hypertensive heart disease with depressed systolic function (mean: 11.05; p= 0.000) than in those who did not develop it. The optimal cutpoint was seven (sensitivity: 92.2 {IC: 88.94 to 95.42}; specificity: 86.7 {IC: 81.67 to 87.17}; validity index 86.7 {IC: 84.55 to 88.85}). External validity. The index showed excellent discriminative ability (area under the ROC curve of 0.954), and the calibration was adequate (Hosmer and Lemeshow: X2= 3.485; p= 0.900). The index obtained for the prognosis of hypertensive cardiopathy evolutionary changes from normal ejection fraction to cardiac insufficiency with reduced ejection fraction has an adequate predictive capacity and calibration, as well as accuracy and reliability.
Keywords: hypertension, hypertensive cardiopathy, prognostic factors, prognostic index.
INTRODUCTION
In 2002 was demonstrated that the relationship between arterial blood pressure and cardiovascular and renal complications is continuous. This fact suggests that the distinction between arterial normotension and hypertension based on arterial blood pressure cut values is somewhat arbitrary1,2,3.
Nevertheless, these arterial blood pressure cut values are helpful in clinical practice for several reasons, among which stand out the necessity of simplifying the diagnosis and decision-making about treatment.
Within this range of target organ damage caused by HT, hypertensive heart disease stands out, defined as a complex and variable set of effects that cause in the heart the chronic elevation of blood pressure and is characterized by anatomical or biochemical signs, or even both of left ventricular hypertrophy or diastolic or systolic ventricular dysfunction, of myocardial ischemia and heart rhythm disturbances4,5.
It is essential to point out that arterial hypertension seldom appears alone since it is frequently associated with a group of cardiovascular risk factors. This aspect increases the probability of cardiovascular complications. Identifying these factors makes possible the stratification of risk of people who suffer from this condition6,7,8.
Despite the new diagnostic and therapeutic developments in hypertensive cardiopathy and the increasing number of studies about the prognosis of this condition, it is necessary to continue researching the topic due to its high prevalence and an increase in the mortality and impairment of patients.
Likewise, it is not known whether an index based on prognostic factors can estimate the evolution of hypertensive cardiopathy with mild diastolic dysfunction to depressed systolic function.
In the present study, we hypothesized that an index based on factors specific to HT, comorbidity and biological markers could predict the evolution of hypertensive heart disease with mild diastolic dysfunction to depressed systolic function.
In answer to the stated hypothesis, the research aimed to evaluate the ability of an index based on prognostic factors to predict the progression of hypertensive heart disease with mild diastolic dysfunction to depressed systolic function.
MATERIALS AND METHODS
Methodological Design
We carried out a prospective cohort study in patients with hypertensive cardiopathy, followed at the specialized arterial hypertension physician’s office of the Specialty Policlinic attached to «Carlos Manuel de Céspedes» General University Hospital, Bayamo Municipality, Granma Province, Cuba. The period evaluated was from Jan 1, 2008, to Dec 31, 2021. The patients followed had at least four appointments per year.
Inclusion and exclusion criteria
Patients over 20 years diagnosed with essential hypertension and grade I hypertensive cardiopathy (diastolic dysfunction without left ventricular hypertrophy diagnosed by echocardiogram) was included. The diagnosis and classification of arterial hypertension were based on the Seventh Report of High Blood Pressure1.
Patients with ischemic cardiopathy were excluded from the research. Despite its high frequency in hypertensive patients and is one of the main causes of cardiac insufficiency, the present study aimed to evaluate the isolated effects of arterial hypertension; therefore, including patients with con ischemic cardiopathy could bias the results. For the same reason, patients with interventricular and auriculoventricular conduction disorders were excluded.
Likewise, it was decided to exclude patients with systemic diseases who, due to their natural evolution or the use of different drugs in their treatment, might cause structural cardiopathies such as thyroid diseases, chronic bowel inflammatory disease, collagen disease, cancer or any other disease that for their characteristics could cause cardiopathy. Patients who had received or were being treated with cytostatic agents were also excluded from the study because these drugs can cause cardiopathy by structural lesions of the myocardium.
Typical background of patients
The patients included in the cohort were selected from the specialized arterial hypertension physician’s office of the Specialty Policlinic attached to «Carlos Manuel de Céspedes» General University Hospital, followed up for several years before the beginning of the study. The evaluation of the cohort started on Jan 1, 2008.
Each patient was submitted to an initial interview and a thorough physical exam to obtain the necessary information. Clinical evaluations were carried out every six months. They included the analysis of clinical data, whereas echocardiograms and electrocardiograms were done annually, except when the patient’s situation required such studies done at any other time.
During the study, all subjects received an initial uniform medical treatment based on a therapeutic protocol accepted by the Research Ethics Commission of the hospital, taking into consideration the latest scientific evidence about arterial hypertension1. The protocol was updated as new recommendations appeared6,7,9.
Characteristics of the sample
Several years before the beginning of the cohort evaluation, 5019 patients were seen at the doctor’s office. Out of them, 3517 (70. 07%) came from urban areas and 1502 (29. 93%) from rural areas; most of them came from Granma Province (Bayamo, it’s the capital city). Considering the criteria previously mentioned, 2707 patients were included in the study.
During the patients’ follow-up (14 years) by the arterial hypertension doctor’s office, there were 207 deaths by causes other than hypertensive cardiopathy (standing out infections and other cardiovascular conditions including ictus) and 306 dropouts (did not attend appointments anymore, the onset of excludible diseases).
Jan 1, 2008, was defined as zero hours or the beginning of the cohort. Once the cohort was started, it was decided not to include any more patients (closed cohort). Each individual evaluation concluded when the patient developed grade IV hypertensive cardiopathy or at the end of the fourteen-year study period in patients who did not produce the condition.

Figure 1. Sample selection
To create and validate a prognostic index, the sample was divided into two parts; the first part was the developing simple with 1194 patients to choose the items to be included in the index, and it’s weighing out (results already published8). The second part was the validation sample that included 1000 patients. This process was carried out using the algorithm included in the Windows SPSS software (version 25.0).
In the validation sample prevailed, the male sex (50.8%), 60.7% of the patients had salt in their diet, and only 3.7% were alcoholic.
Dependent variable
Two categories were included: developing or not grade IV hypertensive cardiopathy (left ventricular hypertrophy with depressed systolic function). For the diagnosis were considered all the hypertensive patients who met the following criteria 9,10,11:
Grade IV hypertensive cardiopathy: all patients with left ventricular hypertrophy and left ventricle with an ejection fraction under 35% (LVEF: percentage of blood expelled from the ventricle with each heartbeat).
Two cardiologists with 25 years of experience in echocardiography performed the echocardiogram. They were using ASAOTE Caris PLUS equipment based on the guidelines of the American Association of Echocardiography10.
Independent variables: those factors Cox’s proportional regression8 showed to be associated with the development of grade IV hypertensive cardiopathy. They are described below.
Age was quantified in years. Patients over 60 years were considered exposed.
The smoking habit was grouped into two categories: smokers (exposed) if they smoked daily or nearly daily cigarettes, cigars or pipes, no matter the number smoked, and ex-smokers for less than a year. Nonsmokers were those who were not in the habit or had quit it for over a year.
Obesity was established by calculating the body mass index (BMI: weight in kilograms divided by size in square meters). Every subject with a muscular mass index greater or equal to 30 or with a waist circumference greater or equal to 102 centimeters for men and 88 centimeters for women was considered exposed.
The biological markers selected were cholesterol, glycemia, C-reactive protein, microalbuminuria and the cholesterol/HDL quotient. The blood samples for each laboratory test were obtained in a fasting state (8 to 12 hours), and were centrifuged at room temperature at 2000 rpm for 10 minutes. Enzymatic methods did all the study determinations.
The cutpoints for the dichotomization of each laboratory variable used in the statistic analysis were established according to a method used to find optimum cutpoints proposed in the literature. The most extreme values on both ends of the variable (under percentile 5 and above percentile 95) were not considered to determine the possible cutpoints.
Likewise, due to the increased probability of type I error when using several hypothesis tests, the following formula was used to correct it: p = −3.13 pmin (1 + 1.65 Ln (pmin)), where pmin is the minimum probability value obtained and p is the corrected value.
The C value was chosen as the optimal cutpoint since it had the highest chi-square result (that is, it was the one with the lowest p-value) for all the values of the dichotomized variables8. In this way, it was selected as a cutpoint for each variable the value that best differentiated patients who developed grade IV hypertensive cardiopathy from those who did not.
In this way, the cutpoints were established, which defined the «exposed» cases at the following values: serum cholesterol more significant than 4.8 mmol/l, cholesterol/HDL quotient greater than 4 mmol/l, fasting glycemia greater than 5 mmol/l. C-reactive protein was determined using the quantitative turbidimetric determination method. Patients with values over 4 mg/l were considered exposed.
Patients with microalbuminuria were considered exposed when their figures ranged from 0. 02 to 0. 2 g/l in 24 hours12, and it was quantified using the Microalb-Latex technique (consisting in the measurement of this substance in the morning first urine void.
During the first year of patient follow-up, they attended three appointments to obtain the quantitative variables’ values (mean of the three results).
Control of HT. Controlled patients were those with blood pressure readings below 140 and 90 mmHg (systolic and diastolic, respectively) in 100% of the HT determinations during each year of follow-up (at least four resolutions per year), complying with optimal medical treatment according to the protocol. Those who did not meet the above criteria were considered not controlled12.
Other blood pressure determinations during other contacts with the health system for whatever reason out of the hospital doctor’s office were also taken into consideration (for this purpose, the patients were instructed to bring in writing their blood pressure values); to guarantee the authenticity of this variable each patient was given a form demanding the following information: date, time, blood pressure values, and doctor’s signature and seal. This document should be presented to the hypertension specialist on the day of the follow-up appointment.
The time of evolution and the hypertension stage were also considered. Concerning the time of evolution, the patients were grouped into two categories: patients with a time of evolution between 5 and 14 years (non-exposed), and patients with a time of evolution equal to or greater than 15 years (exposed). The hypertension stage was classified according to the HTN 7th report proposal, considering the measures proposed for the correct classification and blood pressure determination1.
For the blood pressure determinations, aneroid and mercury sphygmomanometers were previously calibrated by the Territorial Quality and Normalization Office, accredited in Cuba.
Chronic renal disease was also considered (patients in the terminal stage were excluded) as a kidney structural or functional lesion, shown by damage markers (urine, blood or images), independent of the cause that provoked it, for a period equal to or greater than three months14.
To diagnose diabetes mellitus, independent of its type, up-to-date diagnostic criteria were considered15.
The data were obtained in the different appointments using interviews conducted by the authors with the patient’s previous knowledge and consent.
Bias control
To increase the precision and accuracy of the necessary data for the study the following biases were considered:
Selection biases: the out-patient clinical history was used to minimize memory use. Two authors interviewed each patient separately, and their results were compared later. Structured questionnaires were applied to make the interviews more homogeneous.
Information biases: control of these biases was achieved using validated measurement instruments and standardized criteria for sample collection.
Accuracy biases: the data were processed by the authors, and an extrinsic biostatistician and the results obtained coincided.
Adequate data processing was guaranteed with quality control.
Statístic analysis
The statistic analysis started with sample characterization (validation) and the description of all the variables. The means and standard deviations for the quantitative variables were described, as well as the minimum and maximum values for each distribution.
For the comparison of the samples of developing processes 8 and validation, Pearson’s chi-square was calculated for the qualitative variables and the Student’s t test for was calculated for the quantitative variables provided that there was a normal distribution (evaluated by the determination of Kolmogorov-Smirnovy normality test, Levene’s variance homogeneity test) Mann Whitney’s U for those quantitative variables whose distribution was different to normal. The analysis made it possible to evaluate whether there were significant differences between the two samples.
Index construction
It was considered that the index should contain items that could be integrated into a global index that would take the form of a linear combination between the items: I= W1X1+W2X2+……+ WKXK.
Xi is the i-esimal variable to constitute a risk factor in each statistic analysis, and Wi is the «weight» chosen for that variable. Thus, selecting the items that would make up the indicator was considered for the construction stage.
The index was derived from a Cox’s proportional regression analysis of a cohort carried out previously in the same population where the sample was obtained (for ten years)8 taking the cutpoints which would make the greater contribution to the model and that, at the same time, was clinically significant. Each variable ascribed to the model was assigned a score based on the hazard rate (HR) value and approximated to whole numbers. Later, the hazard was classified on an ordinal scale by dividing the index distribution into four zones delimited by the percentiles 10, 50 and 90. In this way, a risk index was proposed. It can be described as an ordinal variable with four categories from minor to significant risk (category I {low}: 0 to 3 points; category II {moderate}: 4 to 6 topics; category III {high}: 7 to 9 points; category IV {very high}: 10 to 19 points).
Index internal validation. Once the index had been constructed, the predictive capacity was calculated: sensitivity, specificity, false positive rate (1- Specificity), positive predictive value, negative predictive value, the positive and negative likelihood ratio and the overall accuracy of the test. We also determined the Youden index to evaluate the optimal cut-off point (it allowed us to classify its performance: sensitivity + specificity – 1).
Index external validation. Its content, presentation, construction and criterion validity were evaluated.
Content and presentation validity:
Expert consultancy. Out of 35 possible experts examined 10 of them were selected, using the preference qualymetric method, based on the determination of the expert’s competence and their willingness to cooperate with this study. Based on the K coefficient, the expert’s self-evaluation of the study was used to obtain scores between 0.7 and 1.
Calculation of K coefficient: K= ½ (Kc + ka) for 35 possible experts.
Where Kc is the expert’s knowledge or information coefficient about risk factors for hypertensive cardiopathy, calculated based on the expert’s awareness in a scale from 0 (total unawareness) to 10 (maximum awareness) and then it is multiplied by 0.1.
And Ka is the argumentation or elaboration coefficient of the criteria determined as a result of the addition of the points obtained in a table.
Calculations were made for each case to obtain each expert’s argumentation coefficient, and the 10 experts with the highest competence were chosen. All of them ranged from 0.8 to 1 point, which suggested that their competence levels ranged from medium to high. The remaining 25 candidates whose competence level was lower than 0.8 were excluded. Each expert was consulted individually and anonymously using a guide created for this purpose.
Out of the 10 experts used: five of them were first and second-degree specialists in Internal Medicine. The test was performed by doctors of medical sciences and full professors and researchers with 15 to 25 years of experience in health care, teaching and research.
The experts have consulted anonymously based on their knowledge and experience in HTN. The experts expressed their opinions about the degree of accomplishment of the five basic properties that should be met by indexes16. Each expert was given an information gathering form to be filled in accompanied by a written explanation of the meaning of the aspects they were expected to evaluate.
The experts stated their opinions about the degree accomplishment of each element according to 3 possibilities: nothing, moderately or very much. The aspects of being evaluated were: understanding of the different items to be assessed concerning the phenomenon to be measured, whether an index can be derived that distinguishes the different prognostic categories if the presence of each item in the instrument is justified16.
Construction validity: to evaluate this indicator, it was taken into account that the greatest morbidity corresponded to patients classified in the highest risk categories. The association between the ordinal index and the risk of developing grade IV hypertensive cardiopathy was evaluated based on calculating the coefficient of association for ordinal and nominal variables, Eta. The comparison of the average index values among patients with grade IV hypertensive cardiopathy and without it was determined using the Student’s t-test for independent samples.
Index discrimination capacity and calibration
Data analysis permitted to obtain of the data for the construction of the ROC (Receiver Operating Characteristics) curve and to determine the index discriminative capacity. A value under the area of the ROC curve greater or equal to 0.7 indicates good discrimination capacity17,18.
Calibration was also estimated employing the Hosmer and Lemeshow test, with a contrast of 10 cutpoints among the observed and expected results. A test value greater than 0.05 means a good calibration.
Accuracy and exhaustiveness determination
Accuracy was calculated to estimate if the positive predictions obtained with the index were correct; also, exhaustiveness was determined to identify whether any bias was present in positive or negative values. High values in both measurements guarantee that the model does not introduce any bias toward positive or negative classes, respectively.
The Gine index was used as a complement to determine the index score differences between the patients with a bad prognosis (evolution to hypertensive cardiopathy with depressed systolic function) and those with favorable evolution.
The Kolmogorov-Smirnov test was used to contrast whether the observations would reasonably result from the specified distribution.
Internal reliability and consistency
It was obtained by determining the Agreement among ten doctors who acted as «judges» and applied the instrument separately to the forms used for the validation sample. The low correlation coefficients for all the possible pairs of judges were obtained. The association between the index categories and the probability of developing hypertensive heart disease was determined by the Kappa coefficient by more than two judges and the Kappa coefficients for each level. Statistical significance was calculated by categories for global Kappa and for each individual Kappa.
The reliability coefficients R and R2 were also determined to know how much of the total variation was due to the patients. Finally, the general Cronbach’s alpha coefficient and the standardized alpha were used to evaluate internal consistency.
Ethical considerations
In the present study, the fundamental ethical principles of clinical and epidemiological research processes for observational studies were met. The Board of Directors and the Ethics Committee of the hospital gave their approval for the study. Potentially eligible patients were informed about the study, and their written consent was obtained. They were also guaranteed that their personal identity and data would not be disclosed. The patients also received appropriate treatment for their condition during the time that the study lasted. None of the patients declined to participate in the study.
Statistical processing was done using the Windows SPSS (version 25.0) computer software.
RESULTS
The index was validated in 1000 patients from a 14-year follow-up cohort. Its baseline characteristics are shown in Table 1.

Table 1. Sample characterization. Baseline values.
Table 2 shows the comparison between both samples (development8 and validation) and no significant differences were found.

Table 2. Comparison of developing samples and index validation.
The index was constructed through a variable selection process and their punctuation, based on the results obtained from Cox’s proportional regression (data published in the Mewade Journal)8. For this purpose, the HR values approximated to whole numbers were used (Table 3).

Table 3. Results of the application of Cox’s proportional multivariate model.
Table 4 shows the index with each of the items and their weighing-out. It also presents the four risk categories, showing high morbidity in categories III and IV. This fact should be highlighted since it indicates that the index permits a good classification of the patients with the worst prognosis¸ so much so that out of the patients classified in category IV, 86.66% developed hypertensive cardiopathy with depressed systolic function.

Table 4. Prognostic index of hypertensive cardiopathy evolutionary changes: diastolic dysfunction to depressed systolic function.
The average values of the proposed index were significantly higher (p= 0.000) in patients who developed hypertensive cardiopathy with depressed systolic function (mean: 11.05) than those who did not (mean: 4. 61).
The internal index validation is represented in Table 5. The optimal cutpoint was seven (sensitivity: 92.2 {CI: 88.94 to 95.42}; specificity: 86.7 {CI: 81.67 to 87.17}; validity index de 86.7 {CI: 84.55 to 88.85}). However, cutpoint 10 was the one that showed the best positive plausibility rate, which means that the probability of a patient classified as high risk to develop hypertensive cardiopathy with depressed systolic function is 30 times greater than in patients classified with lower risk. The Youden index shows that the test output is adequate, where the optimal cutpoint was 7 (Youden index: 0.77; CI: 0.73 to 0.81).

Table 5. Cutpoints of the prognostic index of hypertensive cardiopathy evolutionary changes: diastolic dysfunction to depressed systolic function. Internal validity.
External validation
The index components were submitted to the specialists’ consideration for the analysis of presentation and content validity. It stands out that 90% stated that the content was derivative from the obtainable data and that the components had been clearly defined. 80% of them agreed that the index items were utterly justifiable.
The construction validity (Table 6) was demonstrated by the Eta coefficient value (0.720). 96.58% of the patients with hypertensive cardiopathy with depressed systolic function were classified in categories III and IV.

Table 6. Relationship between the index categories and the risk of hypertensive cardiopathy and depressed systolic function.
Figure 2 shows that the index discriminating capacity was excellent, with an area under the ROC curve of 0.954.

Figure 2. Prognostic index of hypertensive cardiopathy evolutionary changes: diastolic dysfunction to depressed systolic function. Evaluation of the index discriminative capacity.
Table 7 shows that the index has an adequate calibration (Hosmer and Lemeshow: X2= 3.485; p= 0.900) where there was a matching relationship between observed and expected cases in all risk levels.
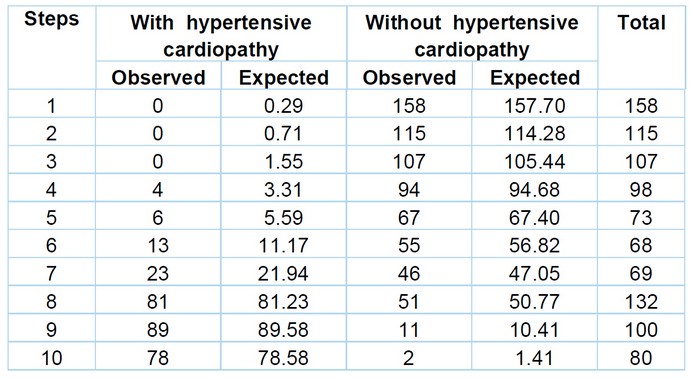
Hosmer and Lemeshow Test: Chi-square: 3.485; p= 0.900
Table 7. Prognostic index of hypertensive cardiopathy evolutionary changes: diastolic dysfunction to depressed systolic function. Calibration.
The index accuracy was evaluated in Figure 3; for cutpoint 7, accuracy was 0.711 and an exhaustivity of 0.922. The Gini index was 0.908, showing the index score differences (high) between the patients with bad prognosis (evolution to cardiopathy with depressed systolic function) and those with favorable development. The Kolmogorov-Smirnov test (0.766) demonstrated that the observations could reasonably come from the specified distribution.

Figure 3. Prognostic index of hypertensive cardiopathy evolutionary changes: diastolic dysfunction to depressed systolic function. Evaluation of the index accuracy.
The reliability coefficient (R) value showed that the major part of the index variation was significantly due to the patients (R= 0.903; p=0.000). Correlation coefficients for all pairs of observers were 0.949 or higher and statistically significant (p: 0.000). Agreement was demonstrated in the 10 pairs of «judges» for all the categories (all of them over 0), the global kappa coefficient was 0.979 (p: 0.001).
The Cronbach’s alpha coefficient to evaluate internal consistency was adequate (0.811). None of the items had values under 0.35, which shows that the index items measure what is intended to be reckoned with them.
Finally, the determination coefficients (R2) were also calculated as part of this process. As seen in Table 8, there was an excellent correlation between each item and the rest.

Table 8. Elements of internal consistency for the simple index through correlation and determination coefficients.
DISCUSSION
Hypertensive cardiopathy is one of the lesions to target organs caused by arterial hypertension with high morbidity and mortality; hence, a correct stratification of its prognosis is significant but, at the same time, a complex task.
As a matter of fact, in the natural evolution of hypertensive cardiopathy, some changes range from a standard or lightly depressed ejection fraction to a cardiac insufficiency with reduced ejection fraction, and it is precisely this evolutionary change the that renders the worst prognosis in comparison with patients who remain stable19.
In the same way, it is a fact that the population aging, the increase of life expectancy and the increment in the prevalence of comorbidities will boost the number of hospitalizations by cardiac insufficiency in the future, perhaps up to 50% in the next 25 years19-21.
For that reason, it is necessary to have tools available that permit to estimate the prognosis of patients with this frequent condition in an objective manner; so with this purpose in mind, the present authors designed an index taking as a point of departure the results previously obtained in a model derived from a Cox’s proportional regression8, which contains 14 items that fitted the context where the studied was done and responded to a probabilistic need of morbidity in vulnerable populations.
The index items and their weighing out are entirely justified from the physiopathological, clinical and practical points of view, as it is evidenced by different studies6-9,19,21-25.
An index based on a cohort has never been used to predict the evolutionary changes of hypertensive cardiopathy from diastolic dysfunction to cardiac insufficiency with a reduced fraction ejection.
In this sense, it should be emphasized that although there are tools available to estimate the risk of dying for patients with acute or chronic cardiac insufficiency24-27, it does not seem advisable to use them to predict the evolution of hypertensive cardiopathy; because even though it shares several prognostic factors, in the present study were evaluated the effects per se of HTN and associated factors which are partially responsible for the structural and functional changes of the myocardium present in the hypertensive patient4,8.
The construction stage showed that the proposed could adequately predict the evolutionary changes of hypertensive cardiopathy; the worst index’s major punctuation will be the prognosis. This aspect is entirely justified by the physiopathologic importance of each item in greater risk 8,19,21-26.
The construction stage showed that the proposed index’s high negative predictive values in each cutpoint indicate that the index ice is unlikely to be classified as low-risk individuals with the worst prognosis. The present study suggests that patients must be classified as high risk from the seven points obtained in the index since the evolution to grade IV hypertensive cardiopathy is very likely. Therefore in these patients, it is paramount to act timely to control or minimize the effects of the factors of the dire prognosis.
For the presentation and content validity, an extensive literature review was carried out, and it was corroborated that the factors considered in the present study are used to predict the evolution of cardiovascular diseases and others are considered important markers of risk of dying1,7-11,13-15 nowadays.
This process may be challenging to evaluate, but clearly defined variables were selected for the index, and experienced professionals in the field were used. It was taken into account that an expert in the topic may point out a relationship between what the study mastery represents for him and the items contained in the indicator16. The result of this study was considered adequate.
In addition, there is a strong relationship between the worst prognosis and the categories of the proposed index, as demonstrated by the values of the Eta coefficient ( worst prognosis in the patients classified in categories III and IV); although they do not reflect the exact value of the prognosis, they are considered acceptable, easy to use and reproduce; in addition, the variables and their selected values are reasonable and are based on the pathogenic importance of each of the factors quoted in the literature2-4,7-9,19-24.
The index discriminative capacity and its calibration show that a tool could identify patients with the worst prognosis better than chance. Undoubtedly, the index can assign the correct result to a couple of subjects selected at random; that is, it permits the classification of the issues in the context of appraisal criterion with binary prediction. In this sense, it should be emphasized that the results mentioned above have a pathogenic base centered on the factors that point to the worst prognosis8,19,22-25.
The proposed index also disclosed adequate accuracy and exhaustivity since it was shown that the patients with the worst prognosis always had higher scores. The results of this study have discarded the existence of a significant error in the classification of patients that would suggest avoiding its use in medical practice.
The correlation coefficients obtained with the Agreement between judges and the kappa coefficient were adequate according to the literature28-30. They reveal that after a short training period, the doctors assisting patients with hypertensive cardiopathy can use the index to predict the evolutionary changes of hypertensive cardiopathy with minimum error. It is essential to point out that these coefficients are very high for categories III and IV, which is very relevant because these patients are precisely the ones who need a better classification.
The internal consistency of the index was shown with the value reached by Cronbach’s Alpha coefficient (according to different studies31-33). Each of the items used in the index measures what is really intended to be measured by them; that is, they can be used to predict the evolutionary changes of hypertensive cardiopathy with mild diastolic dysfunction to depressed systolic function.
The elements of statistical reference of the proposed index have proved to have a high predictive capacity based on their good discrimination and calibration, as well as their internal consistency, showing feasibility and safety for its use in medical practice.
The proposed index uses variables that are available in doctors’ offices, and this makes possible its application in the management of hypertensive patients. In addition, it can be used quickly and economically and provides risk categories with an acceptable performance that can impact decision-making and the patient’s final clinical result.
It should be insisted that the estimation of the prognosis of hypertensive cardiopathy is complex. Despite the new treatments, many patients end up with terminal cardiopathy. Therefore, we must use tools like the one we are proposing to objectively evaluate the medical care provided to hypertensive patients in general and hypertensive cardiopathy patients in particular.
CONCLUSIONS
In short, with the present study, we propose an index to predict the evolutionary changes of hypertensive cardiopathy with mild diastolic dysfunction to cardiac insufficiency with reduced ejection fraction Based on previous research8. The adequate predictive capacity, calibration, accuracy and reliability suggest that the index can be used as a clinical and epidemiological surveillance instrument by identifying the subjects with the worst prognosis.
Novelty and limitations. The novelty resides in the fact that the proposed index is unique. It does not improve or perfect any existing index on cardiac insufficiency. It personalizes the patient’s evaluation and involves only one cardiovascular event (hypertensive cardiopathy). It is not one more general model than the different ones previously published.
Its limitation, however, is that its application in managing hypertensive patients will depend on the doctors’ skills to make good use of it.
Interest conflict statement: the authors deny any conflict of interest.
Funding:The authors claim that there were no external funding sources.
Acknowledgments: The authors acknowledge the invaluable contributions of the Clinical Laboratory and the Imaging and Cardiology Departments.
Claimer: the authors state the availability of data delivery upon request of the editorial committee.
REFERENCES
1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec;42(6):1206-52. doi: 10.1161/01.HYP.0000107251.49515.c2. Epub 2003 Dec 1. PMID: 14656957.
2. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002 Dec 14;360(9349):1903-13. doi: 10.1016/s0140-6736(02)11911-8.
3. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016 Mar 5;387(10022):957-967. doi: 10.1016/S0140-6736(15)01225-8. Epub 2015 Dec 24. PMID: 26724178.
4. Díez J, Frohlich ED. A translational approach to hypertensive heart disease. Hypertension. 2010 Jan;55(1):1-8. doi: 10.1161/HYPERTENSIONAHA.109.141887. Epub 2009 Nov 23. PMID: 19933923.
5. Álvarez-Aliaga A, Quesada-Vázquez AJ, Suárez-Quesada A, del Llano Sosa D. Design and validation of an Index to predict the development of Hypertensive cardiopathy. J Cardiol Cardiovasc Med. 2018; 3:008-022. https://doi.org/10.29328/journal.jccm.1001022.
6. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May 3;79(17):e263-e421. doi: 10.1016/j.jacc.2021.12.012. Epub 2022 Apr 1. PMID: 35379503.
7. Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. Guía ESC 2021 sobre la prevención de la enfermedad cardiovascular en la práctica clínica: Con la contribución especial de la European Association of Preventive Cardiology (EAPC). Rev Esp de Cardiología. 2022; 75(5):429.e1-429.e104. https://doi.org/10.1016/j.recesp.2021.10.016
8. Álvarez-Aliaga A, Frómeta-Guerra A, Suárez-Quesada A, del Llano-Sosa D, Berdú-Saumell J, Lago-Santiesteban YA. Prognostic model of the adaptive changes from hypertensive cardiopathy: from mild diastolic dysfunction to depressed systolic function. Medwave2020;20(3):e7873. Doi 10.5867/medwave.2020.03.7873.
9. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339.
10. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ; Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005 Dec;18(12):1440-63. doi: 10.1016/j.echo.2005.10.005. PMID: 16376782.
11. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W; American Society of Echocardiography’s Nomenclature and Standards Committee; Task Force on Chamber Quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr. 2006 Mar;7(2):79-108. doi: 10.1016/j.euje.2005.12.014. Epub 2006 Feb 2. PMID: 16458610.
12. Pérez Caballero MD, Dueñas Herrera A, Alfonso Guerra JP, Vázquez Vigoa A, Navarro Despaigne D, Hernández Cueto M, et al. Hipertensión arterial. Guía para la prevención, diagnóstico y tratamiento. Comisión Nacional Técnica Asesora del Programa de Hipertensión Arterial. La Habana: Editorial Ciencias Médicas; 2008.
13. Zhao W, Hasegawa K, Chen J. The use of food-frequency questionnaires for various purposes in China. Public Health Nutr. 2002 Dec;5(6A):829-33. doi: 10.1079/phn2002374. PMID: 12638592.
14. Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005 Jun;67(6):2089-100. doi: 10.1111/j.1523-1755.2005.00365.x. PMID: 15882252.
15. Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, et al; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003 Nov;26(11):3160-7. doi: 10.2337/diacare.26.11.3160. PMID: 14578255.
16. Moriyama IM. Problems in the measurement of health status. En: Sheldon EB, Moore W. eds. Indicators of social change: concepts and measurements. New York: Rusell Sage fundation. 1968: 573-99.
17. Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996 Feb 28;15(4):361-87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. PMID: 8668867.
18. Steyerberg EW. Clinical prediction models: a practical approach to development, validation, and updating. Springer; 2009:255-79. https://doi.org/10.1111/j.1751-5823.2009.00085_22.x
19. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. Guía ESC 2021 sobre el diagnóstico y tratamiento de la insuficiencia cardiaca aguda y crónica. Rev Esp Cardiol. 2022;75(6):523.e1–523.e114. https://doi.org/10.1016/j.recesp.2021.11.027.
20. Savarese G, Lund LH. Global Public Health Burden of Heart Failure. Card Fail Rev. 2017 Apr;3(1):7-11. doi: 10.15420/cfr.2016:25:2. PMID: 28785469; PMCID: PMC5494150.
21. Al-Mohammad A, Mant J, Laramee P, Swain S; Chronic Heart Failure Guideline Development Group. Diagnosis and management of adults with chronic heart failure: summary of updated NICE guidance. BMJ. 2010 Aug 25;341:c4130. doi: 10.1136/bmj.c4130. Erratum in: BMJ. 2018 Sep 26;362:k4080. PMID: 20739363.
22. Gorostidi M, Gijón-Conde T, de la Sierra A, Rodilla E, Rubio E, Vinyoles E, et al. Guía práctica sobre el diagnóstico y tratamiento de la hipertensión arterial en España, 2022. Sociedad Española de Hipertensión – Liga Española para la Lucha contra la Hipertensión Arterial (SEH-LELHA) [2022 Practice guidelines for the management of arterial hypertension of the Spanish Society of Hypertension]. Hipertens Riesgo Vasc. 2022 Oct-Dec;39(4):174-194. Spanish. doi: 10.1016/j.hipert.2022.09.002. Epub 2022 Sep 22. PMID: 36153303.
23. Schulz R, Heusch G. C-reactive protein: just a biomarker of inflammation or a pathophysiological player in myocardial function and morphology? Hypertension. 2011 Feb;57(2):151-3. doi: 10.1161/HYPERTENSIONAHA.110.165837. Epub 2011 Jan 10. PMID: 21220709.
24. Huang Y, Wang HY, Jian W, Yang ZJ, Gui C. Development and validation of a nomogram to predict the risk of death within 1 year in patients with non-ischemic dilated cardiomyopathy: a retrospective cohort study. Sci Rep. 2022 May 20;12(1):8513. doi: 10.1038/s41598-022-12249-7. PMID: 35595787; PMCID: PMC9123170.
25. Selvaraj S, Claggett B, Pozzi A, McMurray JJV, Jhund PS, Packer M, et al. Prognostic Implications of Congestion on Physical Examination Among Contemporary Patients With Heart Failure and Reduced Ejection Fraction: PARADIGM-HF. Circulation. 2019;140(17):1369-1379. doi: 10.1161/CIRCULATIONAHA.119.039920.
26. Simpson J, Jhund PS, Lund LH, Padmanabhan S, Claggett BL, Shen L, et al. Prognostic Models Derived in PARADIGM-HF and Validated in ATMOSPHERE and the Swedish Heart Failure Registry to Predict Mortality and Morbidity in Chronic Heart Failure. JAMA Cardiol. 2020 Apr 1;5(4):432-441. doi: 10.1001/jamacardio.2019.5850.
27. Voors AA, Ouwerkerk W, Zannad F, van Veldhuisen DJ, Samani NJ, Ponikowski P, et al. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur J Heart Fail. 2017;19(5):627-634. doi: 10.1002/ejhf.785.
28. Feinstein AR, Cicchetti DV. High Agreement but low Kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543-9. doi: 10.1016/0895-4356(90)90158-l. PMID: 2348207.
29. Streiner DL, Norman GR. ‘Measuring change’, Health Measurement Scales: A practical guide to their development and use , 4th edn (Oxford,2008;online edn,Oxford Academic , Sept 1 2009), https://doi.org/10.1093/acprof:oso/9780199231881.003.0011.
30. Jiménez RE, Vázquez J, Fariñas H. Construcción y validación de un índice de gravedad de la enfermedad para pacientes hospitalizados en áreas clínicas. Gac Sanit [Internet]. 1997 [citado 24 Feb 2009]; 11:122-30. Available at: http://www.elsevier.es/es/revistas/gaceta-sanitaria-138/construccion-validacion-un-indice-gravedad-pacientes-hospitalizados-13141136-articulo-1997.
31. García Cadena CH. La medición en las ciencias sociales y la psicología, en estadística con SPSS y metodología de la investigación de René Landeros Hernández y Mónica T González Ramírez. México, Trillas (comp). 2006.
32. Soler Cárdenas Silvio F. Coeficientes de confiabilidad de instrumentos escritos en el marco de la teoría clásica de los tests. Educ Med Super [Internet]. 2008 Jun [citado 2022 Dic 10] ; 22( 2 ). Available at: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-21412008000200006&lng=es.
33. García-Vargas MLE., Martínez Ayala L, Cerón-Reyes MG, Molina-RuizHD. Validez y confiabilidad de un instrumento que permite detectar una revista depredadora. TEPEXI Boletín Científico De La Escuela Superior Tepeji Del Río. 2022;9(18):9-14. https://doi.org/10.29057/estr.v9i18.8744.
Received: 2 January 2023/ Accepted: 130 March 2023 / Published:15 June 2023
Citation: Álvarez-Aliaga A, Naranjo Flores L L, Suárez-Quesada A, del Llano-Sosa D S, Quesada Vázquez A J, Frómeta Guerra A. Prognostic index of hypertensive cardiopathy evolutionary changes: from mild diastolic dysfunction to depressed systolic function. Revis Bionatura 2023;8 (2) 10. http://dx.doi.org/10.21931/RB/2023.08.02.10


















