Vol 8 No 3 2023 – 24

Efficacy of Health Belief Model in Enhancing Early Detection Behaviors to Prevent Diabetes Mellitus among Mosul University Employees: A Randomized Controlled Trail

1 Telfer sector for primary health care, Nineveh Health Department, Iraqi Ministry of Health, City of Telfer, Iraq; Email: faroukqaplan92@gmail.com.
2 University of Telafer/ College of Nursing/ Clinical Nursing Department/ Iraq/ Nineveh Governorate/ Telafer City; Email: Mohammed.q.baktash@uotelafer.edu.iq.
* Correspondence: faroukqaplan92@gmail.com
Available from: http://dx.doi.org/10.21931/RB/2023.08.03.24
ABSTRACT
Engagement in diabetes early detection investigations plays a significant role in protecting people from this devastating disease. This study aims to determine the efficacy of the health belief model-based health education in improving diabetes early detection behaviors among Mosul University employees. The study is carried out by employing a randomized controlled trial approach and through the recruitment (of 81) individuals from Mosul University employees by adopting a multistage sampling method. The selected subjects were randomly divided into two groups: the experimental group (41) subjects and the control group (40) subjects. A constructed questionnaire is used thrice to gather participants’ data (T0, T1, and T2). A Mixed-design split plot ANOVA was calculated to determine the significance of differences in the participants’ belief scores among groups over time. The study revealed that the sample’s age (M±SD) is (45.26 ± 8.59). In addition, the results show that most of the participants are male (59.3%) and hold bachelor’s degree certificates (40.7%).
On the other hand, the study indicated that the four health belief model concepts of seriousness, susceptibility, benefits, and barriers were significantly changed among experimental group participants after education p ˂ 0.001. As the first study conducted in Iraq, this experiment possesses significant importance. It has been considered a preliminary step to conduct other studies regarding the role of health beliefs in shaping diabetes-protective behaviors among the Iraqi population. The study tested the ability of the health belief model-based- health education to enhance participants’ beliefs regarding diabetes early detection investigations.
Keywords: Health Belief Model, Early Detection, Diabetes Miletus, Health Education
INTRODUCTION
Diabetes is a severe clinical disease that kills many people and possesses a profound biopsychosocial burden1. Statistical data reveals that there were about (537) million people with diabetes in 2021 worldwide, with that figure expected to rise to about (643) million by 2030 and approximately (783) million individuals by 20452. These facts made diabetes prevention a number one public health goal among many countries around the world3.
Numerous factors have motivated public health professionals to concentrate on developing and designing diabetes prevention programs. These factors could be summarized in the considerable expense of diabetes treatment and the clinical nature of the disease (especially type-2)4. Indeed, the natural history of type II diabetes identifies more than ten modifiable risk factors that could be used to eliminate the risk of this terrible condition5.
From another perspective, the maximum advantages of diabetes prevention programs are obtained only by applying them to those at the early stage of the disease6. This illustrates the importance of diabetes early detection measures. However, the only available easy and precise method of diabetes stage determination is by measuring the blood glucose level through several laboratory investigations such as random blood sugar, fasting blood sugar, and hba1c tests 7.
Unfortunately, most people at risk for diabetes do not engage in early detection investigations8. People’s engagement in conducting these tests is controlled by several factors, such as their perception that they are at risk for diabetes and their awareness of the benefits of early detection measures in diabetes prevention9.
The health belief model is one of the famous social cognition models that public health care workers use to educate people about health and disease prevention10. This model assumes that people’s willingness to adopt a disease prevention behavior like engagement in diabetes early detection investigations is influenced by their perception of the severity and susceptibility to disease and the benefits and barriers to the disease prevention behaviors. This study tries to determine the efficacy of HBM-based health education in enhancing diabetes early detection behaviors among Mosul University employees.
MATERIALS AND METHODS
To estimate the efficacy of the health belief model-based health education in enhancing diabetes early detection behaviors among University of Mosul employees, this study employed an experimental design with a randomized controlled trialed approach. The study was conducted in Iraq, Nineveh governorate, at Mosul University from 12 January to 28 March 2022.
Sampling
A multistage random sampling method is employed in this study. The first stage of the sampling process included a random selection of five colleges from the University of Mosul. This procedure is performed by assigning a specific number for each college in the University and then randomly selecting five of them by using the statistical package for social science (SPSS) software. This stage of sampling resulted in the participation of the following Mosul University colleges in the study (the College of Education for Girls, the College of Education for Humanities, the College of Arts, the College of Education for Pure Sciences, and the College of Education). The number of employees in these colleges was (750) taken as a sampling frame for the study. The sample size is estimated by using G-Power software with the following parameters (F-Teats ANOVA repeated measure with between interaction, effect size 0.15, alpha error (0.5), and Beta error (0.8). The result of the G-power analysis indicated that the total required estimated sample size is 74 subjects. The second stage involved using simple random sampling methods to select 100 employees from the colleges under study. However, (19) subjects were excluded because either they refused to participate (n =3) or they do not meet the inclusion criteria (n =16). Ultimately, the number of employees who participated in the study was (81).
Randomization
The final stage of the sampling process involved dividing the study sample into two groups: intervention (41) subjects and non-intervention (40) subjects. The sample distribution into groups was performed by assigning a specific number for each participant and obtaining a random allocation number using the Statistical Package for the Social Sciences (SPSS) software.
Data collection and Instrumentation
After obtaining the informed consent from participants, the data for the study is collected by using parts questionnaires as follows:
Part I: This part included questions about participants’ anthropometric, sociodemographic, behavioral habits, and clinical history characteristics.
Part II: This part of the scale was constructed by using four HBM concepts. The scale consisted of 19 questions. The scale items are distributed among four subscales and measured by a 5-point Likert scale ranging from (1) strongly disagree to (5) strongly agree, with a higher score indicating a more positive perception. The validity of the questionnaires was demonstrated by presenting them to (13) experts in the nursing and medical field. On the other hand, the instrument reliability was calculated by collecting data from (10) employees excluded from the study. Cronbach’s alphas determined the Internal Consistency of the study instrument. The overall internal consistency was equal to (0.8). On the other hand, the instrument’s stability is estimated by a test-retest method with a ten-day interval. The questionnaire’s overall stability was acceptable; r=0.79.
Procedures
The study measured participants’ beliefs regarding diabetes investigations thrice (T0, T1, and T2). At baseline (T0 test), the data is collected from study participants to determine the homogeneity of participants’ beliefs between the two groups (Table 1). At (T1), a two-hour HBM-based health education is employed for the intervention group participants. Health education is provided by adopting the lecture method using data showing devices and figures. The lecture on health education contained two sections:
· Section (1) involved information about the definition, pathophysiology, risk factors, and complications of diabetes.
· section (2) included information about the benefits of diabetes early detection investigations in determining of pre-diabetes state and how to eliminate barriers to these investigations.
After two months, another data collection at (T2) is performed. This third test was essential to estimate the efficacy of HBM-based health education in producing contentious enhancement upon participants’ beliefs.
Data analysis
The Statistical Package for Social Science (SPSS) software for Windows Version 25 was used to analyze the data.
RESULTS
Homogeneity of Sociodemographic Characteristics, Beliefs, Behavioral Habits, and Clinical Risk Factors among Study Participations at Baseline (T0) Test
Table 1 shows that the mean ± SD of the participant’s age is (45.26 ±8.59). The overall mean ± SD of participants BMI = (27.82±4.30). Concerning diabetes early detection-related beliefs, the overall mean ± SD of participants’ beliefs about the seriousness of DM is (2.92 ± 0.66), susceptibility to diabetes is (2.65 ± 0.61), perceived benefits of early detection in preventing diabetes are (2.84 ± 0.72). The perceived barrier to early detection is (2.57 ± 0.52). Regarding other characteristics, the table reveals that most participants are male, hold bachelor’s degree certificates, never smoked, and practice physical activity (1-2) times per week. On the other hand, the most frequent risk factors for DM diagnosis among participants are a family history of diabetes, arterial hypertension, and hypercholesterolemia. Finally, Table 1 illustrates no statistically significant differences in the baseline (T0) test of participants’ characteristics and beliefs between groups.

Table 1. Beliefs and Sociodemographic Characteristics of The Study Sample n (81)
Measuring Change in The Health Belief Model Concepts Over Times
As shown in Table 2, the Mean and Standard Deviation of the participant’s diabetes-related beliefs changed over time. A mixed model-split plot ANOVA (mixed ANOVA) is calculated to identify the significance of changes in the study variables. This test (ANOVA) consisted of one within-subject factor (the three times of testing: T 0, T 1, T 2) and one between the subject’s factors (the two levels of groups: Experimental and Control). In this test, the P-value of less than 0.05 was reported as significant for all effects. The analysis indicated that the differences in the study concept’s mean scores are caused by time and that there was no effect for the type of group (condition) or interactions between group type and testing times. Precisely, the table 2 reveals that time has an essential impact on participants perceived seriousness of diabetes, F (2, 79) = 9.265, P < .000, perceived susceptibility to diabetes, F (2, 79) = 27.561, P < .001, perceived benefits of early detection in preventing diabetes, F (2, 79) = 7.868, P < 0.001, perceived barrier to early detection F (2, 79) = 31.678, P = 0.001. On the other hand, the effect size associated with the changed beliefs was identifiable, with time accountable for approximately 10% of the variance from changed seriousness, 25% of the variance from changed susceptibility, 9% of the conflict from changed benefits, and 28% of the variance from changed barriers.
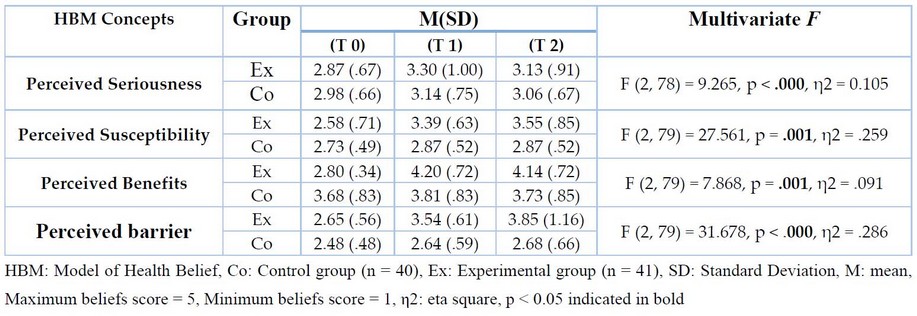
Table 2. Descriptive Statistics and Mixed ANOVA Measuring Changes in The Health Belief Model Concepts Across Study Groups and Over Time.
Determining the Efficacy of Health Belief Model-Based Health Education in Changing Experimental Group Participant’s Beliefs Over Time:
According to the results from (Table 2), the Bonferroni corrections test was essential to calculate as a post-doc test to determine where the differences among participants’ belief mean scores over time exactly lie. The post-doc analysis revealed a significant enhancement in the belief scores of experimental group participants (p < 0.05) over time. Regarding the control group, there was no exact improvement or continuous stable changes among variables over time. These results establish the efficiency of HBM-based health education in eliciting enhancement among participants’ diabetes-related beliefs over time (Table 4).
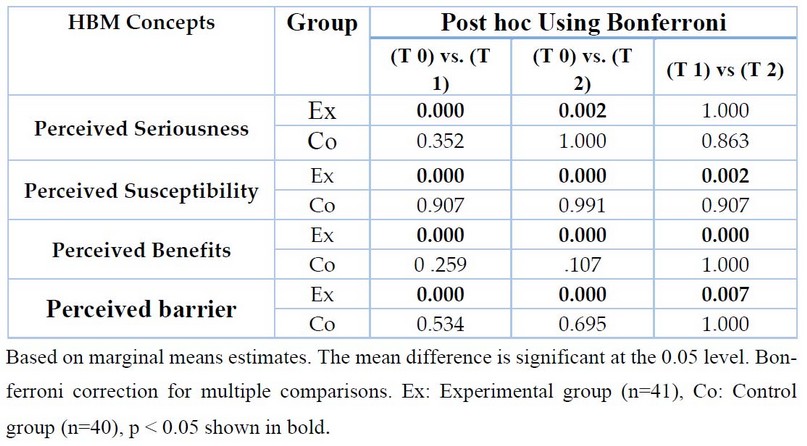
Table 3: Post-hoc Analysis for Health Belief Model Concepts
DISCUSSION
The significance of this study lies in the fact that it is the first scientific experiment trying to enhance diabetes early detection behaviors among employees of the University of Mosul through health education and by adopting one of the most famous social cognition models (The Health Belief Model).
Most participants in the study are in middle adulthood age, overweight, male, hold a bachelor’s degree certificate, never smoked, and perform physical activity 1- 2 times per week (Table 1). These characteristics are consistent with several studies conducted in universities of Iraq and the world(12-14). These studies revealed that most of the university employees are male, in middle adulthood, and hold bachelor’s degree certificates. Regarding clinical diabetes risk factors, Table 1 indicates that family history of diabetes, arterial hypertension, and hypercholesterolemia are the most common clinical risk factors diagnosed among study participants. This result is congruent with the statistical data for the prevalence of diseases in Iraq available on the World Health Organization website. The World Health Organization website illustrates that most diseases prevalent among adults in Iraq are diabetes, stroke, arterial hypertension, and heart disease15.
The participant’s characteristics measurement was essential because the HBM assumes that individuals’ beliefs are influenced by their characteristics16. On the other hand, one of the critical criteria for conducting randomized controlled trial (RCT) studies is the presence of homogeneity between the experimental and control groups. The homogeneity shown in Table 2 among study groups’ demographical characteristics, beliefs, behavioral habits, and clinical history provides feasibility to completing this study.
Concerning health education, Table 3 and 4 shows that HBM efficiently changes many Mosul University employees’ diabetes-related beliefs. These Tables reveal that post-education, the experimental group’s participants felt that diabetes is a serious condition and that their susceptibility to diabetes would be high if they did not engage in diabetes early detection investigations. Further, the participant’s perceived benefits and barriers regarding early detection behaviors were improved dramatically after intervention with health belief model-based health education.
These interpretations of study results prove the capacity of HBM-based health education to change adults’ beliefs regarding diabetes early detection measures.
CONCLUSIONS
As the first study conducted in Iraq, this article possesses significant importance. It is considered a preliminary step to conduct other studies regarding the role of health beliefs in shaping diabetes protective behaviors among the Iraqi population. The study provides clinically significant information about diabetes. It has proved the ability of the health belief model health education to enhance participants’ beliefs regarding diabetes early detection investigations.
Author Contributions: All authors have contributed equally in all study parts. All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding
Institutional Review Board Statement: A thorough adherence to ethical principles, including the 1964 Helsinki Declaration and later additions or adjustments, are applied in this study. The informed concept is obtained from all employees engaged in the study. The study is conducted under the research program of the Nursing College at the University of Mosul.
Informed Consent Statement: Written informed consent has been obtained from the participants to publish this paper.
Acknowledgments: All thanks and appreciation to the University of Mosul and the University staff for helping us obtain the research sample.
Conflicts of Interest: The authors declare no conflict of interest.
REFERENCES
1. Mokabel FM, Aboulazm SF, Hassan HE, Al-Qahtani MF, Alrashedi SF, Zainuddin FA. The efficacy of a diabetic educational program and predictors of compliance of patients with noninsulin-dependent (type 2) diabetes mellitus in Al-Khobar, Saudi Arabia. Journal of family & community medicine. 2017;24(3):164.
2. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes research and clinical practice. 2021:109119.
3. Baker MK, Simpson K, Lloyd B, Bauman AE, Singh MAF. Behavioral strategies in diabetes prevention programs: a systematic review of randomized controlled trials. Diabetes research and clinical practice. 2011;91(1):1-12.
4. Mikhael EM, Hassali MA, Hussain SA. Validation of newly developed culturally specific diabetes self-management education and support program for Iraqi type 2 diabetes mellitus patients. Journal of Education and Health Promotion. 2021;10.
5. Fletcher B, Gulanick M, Lamendola C. Risk factors for type 2 diabetes mellitus. Journal of Cardiovascular Nursing. 2002;16(2):17-23.
6. Nikitara M, Constantinou CS, Andreou E, Diomidous M. The role of nurses and the facilitators and barriers in diabetes care: a mixed methods systematic literature review. Behavioral sciences. 2019;9(6):61.
7. Taylor R, Batey D. Handbook of retinal screening in diabetes: diagnosis and management: John Wiley & Sons; 2012.
8. Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes, metabolic syndrome and obesity: targets and therapy. 2019;12:75.
9. Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. The Lancet. 2014;383(9933):1999-2007.
10. Abraham C, Sheeran P. The health belief model. Predicting health behavior: Research and practice with social cognition models. 2015;2:30-55.
11. Bayat F, Shojaeezadeh D, Baikpour M, Heshmat R, Baikpour M, Hosseini M. The effects of education based on extended health belief model in type 2 diabetic patients: a randomized controlled trial. Journal of diabetes & Metabolic disorders. 2013;12(1):1-6.
12. Andersen J, Wade M, Possemato K, Ouimette P. Association between posttraumatic stress disorder and primary care provider-diagnosed disease among Iraq and Afghanistan veterans. Psychosomatic Medicine. 2010;72(5):498-504.
13. Robinson JK, McMichael AJ, Hernandez C. Transparent reporting of demographic characteristics of study participants. JAMA Dermatology. 2017;153(3):263-4.
14. Ross LE, Campbell VL, Dennis C-L, Blackmore ER. Demographic characteristics of participants in studies of risk factors, prevention, and treatment of postpartum depression. The Canadian Journal of Psychiatry. 2006;51(11):704-10.
15. World Health Organization. Noncommunicable diseases progress monitor 2022. 2022.
16. Fithri R, Athiyah U, Zairina E. The development and validation of the health belief model questionnaire for measuring factors affecting adherence in the elderly with hypertension. Journal of Basic and Clinical Physiology and Pharmacology. 2021;32(4):415-9.
17. Green EC, Murphy EM, Gryboski K. The health belief model. The Wiley encyclopedia of health psychology. 2020:211-4.
Received: 28 May 2023/ Accepted: 15 July 2023 / Published:15 September 2023
Citation: Younus, F.; Baktash, M. Efficacy of Health Belief Model in Enhancing Early Detection Behaviors to Prevent Diabetes Mellitus among Mosul University Employees: A Randomized controlled trial. Revis Bionatura 2023;8 (3) 24. http://dx.doi.org/10.21931/RB/2023.08.03.24



















