Vol 8 No 1 2023 – 90

1 Department of Pharmacology, College of Medicine, University of Al-Iraqia, Baghdad, Iraq; raghad.a.khaleel@aliraqia.edu.iq
2 Departement of Pharmacology and Toxicology, College of Pharmacy, University of Baghdad; munafzalzala@copharm.uobaghdad.edu.iq
3 Council of Arab Board of medical specialties Dermatology and Venereology diseases, Yasirmuslih85@gmail.com
Available from: http://dx.doi.org/10.21931/RB/2023.08.01.90
ABSTRACT
Psoriasis is a chronic, inflammatory condition that primarily affects the skin, hair, and joints and is associated with significant humanistic and economic consequences. This work induced psoriasis in mice using an imiquimod 5% cream, an immune response modifier that can cause psoriasis-like skin inflammation when given orally. Paquinimod is prepared as an ointment and has been topically given to mice before imiquimod application. In this study, albino mice were allocated into five groups and treated as follows: the control group received only a daily application of cream based on shaved back (62.5mg/2cm) with a daily topical dose of ointment for 14 consecutive days with the oral vehicle. The Imiquimod group received a daily topical dose of vehicle one hour before imiquimod 5% application on shaved back (62.5mg/2cm) for 14 consecutive days. The paquinimod-treated group received daily topical doses of paquinimod one hour before imiquimod 5% application on shaved back (62.5mg/2cm) for 14 consecutive days. Clobetasol -treated group received a daily topical dose of clobetasol ointment (62.5mg/2cm) one hour before imiquimod 5% application on shaved back (62.5mg/2cm) for 14 consecutive days. Paquinimod, the only group that received a daily oral dose of paquinimod for 14 consecutive days. The current study found that the administration of paquinimod ointment resulted in a significant decline in TNF-α, IL-23, IL17 level, reduced psoriasis area and severity index, spleen index, skin thickness, and gene expression of TNF-α, Nf-KB, IL-1B, IL-17in the (Paquinimod ointment+imiquimod) group substantially more than that in the (vehicle ointment+imiquimod) groups. In conclusion, paquinimod has a powerful ameliorating effect that can reduce the IMQ-induced psoriasis-like inflammation in a mouse model. As a result, we have every reason to believe that paquinimod will be utilized to treat psoriasis.
Keywords: Psoriasis; Paquinimod; Imiquimod; IL-23; IL-17; TNF-α.
INTRODUCTION
Psoriasis is a well-known chronic inflammatory skin and joint disorder that is often accompanied by emotional and social difficulties that can result in substantial limitations and a poor quality of life. However, because the etiology is still unknown, epidemiological studies have concentrated on determining the pathogenesis contribution, which has revealed predisposing genetic and autoimmune features in the disease process 1-5. The desired goal of psoriasis treatment is to enhance symptom control, improve quality of life, reduce psychiatric comorbidity, and avoid structural damage and impairment. Psoriasis is an immunologically mediated illness in which the activation of T lymphocytes causes dermal inflammation and epidermal hyperproliferation as a result of the inflammatory processes. In patients with well-developed psoriasis, pharmacological treatment of imiquimod (IMQ) has been manifested to activate or aggravate psoriasis.IMQ can cause erythema, acanthosis, and a mixed inflammatory infiltrate of lymphocytes, dendritic cells (DC), and neutrophils in mice like those that happened in psoriasis. Modern studies have shown that the IL-23/Th17 axis, which is essential in the pathogenesis of psoriasis in humans, is also important in the mouse skin inflammation caused by IMQ. Because the expression of IL-23 and Th17-related cytokines are increased in the lesional skin and IL-23 deficiency or blockade suppresses the inflammation, modern studies have shown that the IL-23/Th17 axis, is important. However, the mechanisms of IMQ treatment-induced activation of the IL-23/Th17 pathway and the development of psoriasis-like skin inflammation are yet unknown. Paquinimod interacts with the S100A9 protein and blocks it from interacting with other proteins (RAGE and TLR-4) 6. A new calcium-binding protein that is secreted by stressed cells in necrosis acts as an endogenous danger signal, speeding up and exacerbating the inflammatory response entitled S100A9. Because they block the actions of the calcium-binding protein A9 of S100, quinoline-3-carboxamides take advantage of being used to treat autoimmune and inflammatory illnesses in humans (S100A9). Chemotaxis, neutrophil and macrophage modulation, and inflammatory signaling pathways are all activated by this molecule.
On the other hand, paquinimod (ABR-215757, C21H22N2O3) blocks S100A9 from interacting with RAGE and TLR4. The activation of NKT-II T cells can be also stopped by paquinimod 7. The pathological events of autoimmune/inflammatory disease models such as experimental collagenase-induced osteoarthritis, systemic lupus erythematosus (SLE) patients, and systemic sclerosis all can be reduced by paquinimod. The S100A family proteins have a role in inflammatory reactions by causing proinflammatory cytokines to be produced by a range of immune and non-immune cells, including monocytes, neutrophils, endothelial cells, keratinocytes, and epithelial cells. NKT-II cells are affected by paquinimod, CD4 (+) T cells, CD115+ Ly6Chi monocytes, and CD11b+ F4/80+ CD206+ macrophages become less primed as a result of this 8. In this study, mice were given paquinimod topically before being given imiquimod to cause psoriasis.
MATERIALS AND METHODS
Chemicals and Kits
The chemicals used in this work include formalin (merk chemicals, Germany), diethyl ether (BDH chemicals, India), xanthan as a suspending agent (Samara drug industry Iraq (, Imiquimod cream (MEDA-Germany), Paquinimod (Sigma-Aldrich USA), Clobetasol propionate ointment (GlaxoSmithKline), Dexamethasone syrup (Samara drug industry Iraq), and Dulbecco’s phosphate-buffered saline (Euro Cyclone S.p.A, Italy). The kits used in this study include (Interleukin-23, Interleukin-17, Tumor Necrosis Factor alfa) all of them from (Bioassay technology laboratory, China), also RNA purification kit (GENEzolTM TriRNA Pure Kit, Geneiad, India), gDNA remover, and cDNA synthesis super Mix (Transgen).
Animal Treatment
Forty (40) BALB/c albino mice (male, 8wk) (22-40 g wt.) were kept in pathogen-free environments and given unlimited food and drink. All animal tests were carried out in the Animal House of the University of Baghdad’s College of Pharmacy, and were kept in a 12-hour light-dark cycle with regulated air temperature (15-21 C) and ethical and animal care approval.
Preparation of Paquinimod Ointment
The ointment was prepared by mixing 0.05gm of paquinimod with 0.5ml of liquid paraffin and then completing the weight to 5gm using a Vaseline ointment base. (The final concentration of Paquinimod ointment is 1%) according to British pharmacopeia with the pharmaceutics department help.
Experimental Design
Approximately forty (40) mice were shaved from the back area using a traditional manual eraser (trimming not zero shaving), and all the mice were weighed at zero time.
The mice were put into five groups, each with eight animals:
1. Control group: In which mice were given a topical dosage every day of cream base of imiquimod on shaved back (62.5mg/2cm) for 14 a string of days.
2. Imiquimod group (model group): In which mice were given a topical dosage every day of the base of paquinimod ointment one hour before imiquimod 5% application (62.5 mg / 2 cm) on shaved back for 14 consecutive days.
3. Paquinimod treated group: In which mice were given a topical dosage every day of paquinimod ointment one hour before applying 5% imiquimod (62.5 mg / 2 cm) on shaved back for 14 consecutive days.
4. Group treated with clobetasol propionate: In which mice were given a topical dosage every day of clobetasol propionate daily (0.05%) ointment one hour before applying 5% imiquimod (62.5 mg / 2 cm) on shaved back for 14 consecutive days.
5. Paquinimod-only group: In which mice have received a daily topical dose of paquinimod ointment on shaved back (62.5mg/2cm) for 14 consecutive days. A professional dermatologist determined the psoriasis area and severity index. All mice were weighed before being euthanized at the end of the experiment, and blood was collected for biochemical analysis.
The severity of skin inflammation is graded as follows
The intensity of back skin inflammation was determined using an objective scoring system based on the clinical PASI score. On a scale of 0 to 4, erythema, scaling, and thickness were all graded separately: 0 indicates no, 1 indicates a minor difference, 2 indicates a moderate difference, 3 indicates a significant difference, and 4 indicates a significant difference. The lower the PASI score, the lower the quality of life and the lower the contentment with skin conditions. Similarly, an improvement in the PASI was associated with an improvement in the conventional PASI score for general bodily pain for mice 9.
Measurements of spleen index
All mice were weighed, and when mice were sacrificed, the spleen index is determined by dividing the spleen weight of the mice in mg by body weight in gm 10.
Skin thickness measurements
At the end of the experiment, the skin thickness of the back area was measured in mm via digital Vernier caliper and compared estimated thickness between groups 11.
Assessment of inflammation
Approximately 1 to 1.5 ml of blood was drawn from the retro-orbital vein and placed in an Eppendorf tube before being centrifuged at 3500 rpm for 15 minutes to obtain serum, which was separated and stored at -20 C until the day of analysis. According to the manufacturer’s protocols, serum was used to estimate serum IL-23 and IL-17 levels using ELISA kits 12.
Tissue homogenate
Before homogenization, skin tissue from the back area was thoroughly the samples were washed in PBS (PH7.4) and weighed. To eliminate excess blood,. By homogenizing the tissue in PBS (pH 7.4) homogenizer on ice, and melting at 2-8 ° C or frozen at -20 ° C. Finally, the homogenized tissue was centrifuged at (2000-3000) RPM for approximately 20 minutes 13.
Polymerase chain reaction procedure
Total RNAs were extracted using Trizol from (GENEzolTM TriRNA Pure Kit, Geneiad, India). Reverse transcriptase PCR was accomplished through consecutive standard procedures. The primer pairs of the expected products are shown in table 1. All primers were purchased from Applied Bio systems 14:
A. RNA Purification Protocol Procedure
The sample should be prepared at room temperature.
1. Directly remove 10-50 mg of tissue from the animal or take the tissue sample out of storage.
2. In a 2 ml centrifuge tube containing ceramic beads or stainless steel beads, transfer the tissue and 700 l of GENEzolTM Reagent, then homogenize the sample using a Tissue Lyser, Disruptor Genie, or equivalent.
3. Allow the homogenized sample to incubate at room temperature for 5 minutes.
B. RNA Binding
1. To remove debrided cells, the samples were centrifuged for one minute at 16,000 x g, then the supernatant was transferred to a new microcentrifuge tube (1.5 ml, RNase-free).
2. In GENEzolTM Reagent, absolute ethanol was added immediately (1:1) to the sample combination.
3. A vortex was used to thoroughly mix the sample combination, and then an RB Column was placed in the Collection Tube (2 ml).
4. The 700 l sample mixture was transferred to the RB Column, centrifuged for one minute at 16,000 x g, and the flow-through was discarded.
C. RNA Wash
1. Pre-Wash Buffer (400 l) was added to the RB Column and centrifuged at 16,000 x g for 30 seconds. Replaced the flow-throughs in the Collection Tube after discarding them (2 ml).
2. The Wash Buffer (600 l) was added to the RB Column and the process was repeated.
3. Pre-Wash Buffer (600 l) was added to the RB Column, and the same processor was used again.
4. The column matrix was dried by centrifuging it at 14-16,000 x g for 3 minutes at 16,000 x g.
D. RNA Elution
1. A micro-centrifuge tube (RNase-free, 1.5 ml) was filled with the dry RB Column.
2. RNase-free water (25-50 l) was poured into the matrix center of the column.
3. Wait 3 minutes to check that the RNase-free Water has completely absorbed the matrix.
4. Centrifuge for 1 minute at 16,000 x g to completely elute the pure RNA.
One step gDNA Removal and cDNA Synthesis. The cDNA synthesis was subjected by using the protocol in Easy Script® One-Step gDNA Removal and cDNA Synthesis Super Mix. Procedure:
1. First strand cDNA synthesis.
2. The reaction components and the volume needed are shown in table (2-1).
Incubation: The time and temperature needed to be shown in (2-2).
Histopathological examination
The skin of the back area and the right ear of the mice were removed. After that, the tissue was washed in normal saline solution to prepare it for histological investigation. Tissues were cleansed, and formaldehyde was used to fix them (10 percent of formaldehyde in water). Hematoxylin and eosin stain was used to stain the thin section slide for tissues, which was then mounted with a protective coverslip 15.
Statistical analysis
Data were expressed as mean values (mean standard error of the mean) in statistical analysis (SEM). In this case, a one-way ANOVA analysis was used to see if there was a significant difference between the groups’ means. The variation was considered statistically significant when the P-value was less than 0.05 (0.05).
RESULTS
Topical effect of paquinimod on the PASI score
The PASI score was significantly increased in the (model) animal treated by imiquimod compare to the (control) group. The anti-inflammatory effect of paquinimod successfully decreased the PASI score in comparison to model animals. Clobetasol topical application significantly decrease the PASI score in comparison to IMQ treated group (figure 1).
Effect of paquinimod on the skin thickness
Figure 2 demonstrated that the increase in skin thickness in the (model) group was significantly greater than in the (control) group. Clobetasol and paquinimod treatment resulted in a significant decrease in skin thickness when compared to the IMQ-treated mice group. Skin thickness remains normal in the (Paquinimod oint) group, as it does in the control group.
Effect of topical administration of paquinimod on spleen index against imiquimod-induced psoriasis in mice
Figure 3 shows that the spleen index for mice in the IMQ-treated group was significantly higher than in the control group. When compared to the control group, the spleen index in the (Paquinimod oint + IMQ) group remains roughly normal. While in the Clobetasol-treated group the measured spleen index decreases significantly compared to the (Vehicle oint+IMQ) group.
Effect of topical administration of paquinimod on serum IL-23, IL-17, and TNF-α levels against imiquimod-induced psoriasis in mice
Figure 4 A and B show that there was a significant increase (P<0.05 percent) in serum levels of IL23 and IL-17 in the IMQ-treated group compared to the normal control group, and that clobetasol treatment showed a significant decrease in serum IL23 (P<0.05) compared to the model group. In addition, topical paquinimod administration significantly reduced serum IL-23 and IL-17 levels when compared to the (Vehicle + IMQ) group (P<0.05). The effect of paquinimod oint on serum IL23 and IL-17 levels was significantly lower in comparison to normal mice (P<0.05). Figure 4 C revealed a significant elevation in tissue TNF- level (P<0.05) in the group (Vehicle oint + IMQ) as compared to the normal control group, as well as a significant reduction in tissue TNF- level (P<0.05) in the group (Paquinimod oint + IMQ) group (Vehicle oint + IMQ) group, as well as a significant reduction (P0.05) in the group There was a significant reduction (P<0.05) in tissue TNF- level in the group (Paquinimod oint only) compared to the group (Vehicle oint + IMQ).
Effect of topical administration of paquinimod on gene expression of IL-1B, TNF-α, NF-kB, and IL-17 against imiquimod-induced psoriasis-like inflammation in mice
Figure 5A displayed that gene expression for IL-1B in mice treated with IMQ was highly significantly expressed. The anti-inflammatory effect for paquinimod revealed a significant reduction for IL-1 B’s expression is in comparison to the model group alternatively, the relative level of IL-1B mRNA in skin tissue for mice treated with clobetasol or paquinimod alone showed significant inhibition compared to control mice. In figure 5B, the model mice treated with IMQ have expressed the level for TNF-α in the skin in a highly significant increase than control mice. The gene expression of TNF-α for (Paq. Oint + IMQ) group was significantly reduced compared to the mRNA level for TNF-α in (Vehicle+IMQ) group. On other hand, gene expression of TNFα for mice of (Clobetasol oint+IMQ) and (Paq oint only) groups were showing significantly different compared to gene expression of TNF-α for mice of (Control) group. Figure 5C manifested that the topical administration of paquinimod produces a significant reduction in mRNA level for NF-κB in the skin and inhibits the inflammatory effect for imiquimod. Clobetasol has a clear anti-inflammatory effect on NF-κB level in comparison to the model group. The gene expression for IL-17 in the back skin for the model group was elevated higher than that in the normal animal. Paquinimod successfully reduced the gene expression for IL-17 in comparison to model mice. Clobetasol produce paquinimod like effect on IL-17 level.
-Each value denotes the mean and standard deviation (SD).
– * Significantly different from the control group (P0.05).
– # P<0.05% significant compared to the vehicle oint + IMQ group.
Effect of topical administration of paquinimod on histological examination against imiquimod-induced psoriasis in mice
The histological sections of the normal control group’s skin in the back area had a normal appearance, as shown in Figure 6 A. The histological section of the skin of the back area (vehicle oint + IMQ) showed marked hyperkeratosis and acanthosis (5 cells) of the epidermis with heavy inflammatory cells in the upper dermis, as shown in Figure 6 B. In addition, paquinimod pretreatment resulted in a section of back area skin with a normal-looking appearance of skin tissues, as shown in figure 6 C. The back section of the Clobetasol-treated mice showed a thin epidermis layer, hyperkeratosis with mild acanthosis, and a rete ridge with mild inflammatory cells, as shown in Figure 6.

Figure 1. The area and severity index of psoriasis (PASI) after topical administration of paquinimod in imiquimod-induced psoriasis in mice

Table 1. Reaction Components and volume

Figure 2. Effect of topical administration of paquinimod on skin thickness in imiquimod-induced psoriasis in mice
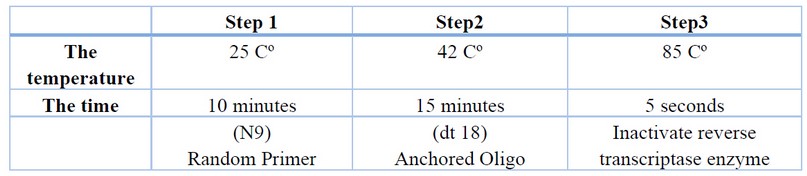
Table 2. Thermal cycler steps

Figure 3. Spleen index after topical administration of paquinimod in imiquimod-induced psoriasis in mice

Table 3. Gene name and primer sequences for products

Figure 4. Effect of topical administration of paquinimod on (A: Serum IL-23 level, B: IL-17 level, and C: TNF-α level) against imiquimod-induced psoriasis in mice

Figure 5. Effect of topical administration of paquinimod on gene expression of IL-1B, TNF-α, NF-ΚB, and IL-17 against imiquimod-induced psoriasis-like inflammation in mice

Figure 6. Effect of paquinimod on IMQ-induced pathological changes in psoriasis on the skin of the back area. Staining: Hematoxylin and eosin (H&E)
Black arrows: Sign of the thickness of the epidermal layer of the right ear section. A: control group; B: Vehicle+IMQ group; C: Paq oint+IMQ group; D: Clobetasol oint+IMQ group; E: Paq oint only group; Histology scoring analysis. Each value represents mean ± SD.
DISCUSSION
Psoriasis is a well-known chronic inflammatory skin and joint disorder that has been linked to emotional and social difficulties, which can result in substantial disability and a decrease in quality of life (1). Imiquimod (IMQ) is a synthetic Toll-like receptor (TLR) 7 agonist used to treat human papillomavirus-caused vaginal and perianal warts, actinic keratosis, and superficial basal cell carcinoma. In the current study, psoriasis-like skin inflammation (erythema, acanthosis, and a mixed inflammatory infiltrate involving lymphocytes, dendritic cells (DCs), and neutrophils) was induced by imiquimod (5). Paquinimod belongs to a class of compounds known as quinoline-3-carboxamide derivatives, which have shown efficacy in treating autoimmune diseases in both humans and mice (10). A designful scoring system was discovered to score the severity of inflammation of the back skin (11). In the current study, the PASI score for the (Vehicle oint+IMQ) group was significantly higher than the PASI score for the (Control) group, indicating that IMQ applied topically caused increased skin inflammation as evidenced by increased skin thickness (12). Paquinimod appears to have significant anti-inflammatory activity in this study, as evidenced by a significant reduction in the PASI score in the (Paquinimod oint+IMQ) group compared to the (Vehicle oint+IMQ) group. Paquinimod acts on the (S100A9) protein and inhibits the binding of (S100A9 to RAGE and TLR-4). A range of autoimmune and inflammatory disorders in humans can be treated by Quinoline 3 carboxamides due to their ability to suppress the actions of the calcium-binding protein A9 (S100A9). The S100A9 can be defined as a tiny calcium-binding protein generated by stressed cells in necrosis that works as an endogenous danger signal for the body’s defenses to ramp up(6). This molecule activates the inflammatory response signaling pathway, causing chemotaxis and neutrophil and macrophage modulation (7). The daily dose of paquinimod resulted in a significant reduction in serum interleukin levels (IL17, IL23), which was revealed by significantly reduced in the group (Paq oint+IMQ) as compared to the (Control) group, indicating that the paquinimod ointment acts as an anti-inflammatory agent by decreasing the serum level of these interleukins. The histological features have been improved as well. Interleukin 23 (IL-23), a cytokine that promotes the formation of IL-17 and IL-22-producing Th17 cells, was assumed to play a direct role in the pathogenesis of psoriasis. In psoriasis lesional skin, IL-23 expression is increased, as are the numbers of Th17 cells. The current study showed a significant increase in TNF- levels after treatment with paquinimod compared to the control group. The induction of TNF- was reduced in the paquinimod-treated group due to its protective effect against imiquimod-induced inflammation. This is consistent with numerous previous studies that found paquinimod to have anti-inflammatory properties 16. TNF- levels were significantly lower in the (Paq oint+IMQ) group compared to the (Vehicle oint+IMQ) group (P-value 0.05 percent). Psoriasis and other chronic inflammatory conditions appear to be caused by an overactive immune system, with the (TNF, type I IFNs, and the IL-23/IL-17) axis all playing intertwined roles 17. An RT-PCR technician could also measure gene expression of tumor necrosis factor-alpha, interleukin 17, interleukin1 beta, and nuclear factor kappa B (TNF, IL-17, IL-1B, and NF-Kb) in mRNA. In this study, a strong positive correlation was found between the gene expression of (TNF, IL-17, IL-1B, NF-kB) and the administration of paquinimod topically, with the expression of the mentioned gene being significantly higher in the (Vehicle oint+IMQ) group compared to the (Control) group. Paquinimod, on the other hand, possesses anti-inflammatory properties that inhibit proinflammatory cytokines like TNF, IL-17, IL-1B, and NF-Kb gene expression 18.
The histopathological testing alimportsort further endorsement for the protective action of paquinimod on psoriasis caused by imiquimod in which the section of the skin tissue of the back area in the (Paquinimod oint+IMQ) group showed a normal-looking appearance and this clearly explained the ameliorating effect of paquinimod as compared with the skin section of the back area in the (Vehicle oint+IMQ) group in which IMQ causes symptoms of local psoriasis recognized by inflammation, agglomeration, and scaling of the skin, hyperplasia of the epidermal layer with the retention of nuclei in the stratum corneum (parakeratosis), a neutrophil-rich stratum corneum (Munro’s abscess), granular epidermal layer thinning, and an infiltrate of the mononuclear dermal and epidermal layers T cell and dendritic cell infiltration in plaques, as well as dysregulated angiogenesis of cutaneous blood vessels, have also been describedn17. The proteins of the S100A family mediate inflammatory reactions by acting on a variety of immune and non-immune cells, including monocytes, neutrophils, endothelial cells, keratinocytes, and epithelial cells, to produce proinflammatory cytokines 7. Furthermore, the Imiquimod-based psoriasis murine model revealed a strong link between the role of NK cells in the pathogenesis of autoimmune diseases like psoriasis and paquinimod, a drug that has been shown to modify NKT-II cells and reduces the priming of proinflammatory effector CD4 (+) T cells, CD115+ Ly6Chi monocytes, and CD11b+ F4/80+ CD206+ macrophage 19-20.
CONCLUSION
In conclusion, the current study found that paquinimod treatment of mice has ameliorative effects against imiquimod-induced psoriasis comparable to clobetasol, with paquinimod being more effective than clobetasol in terms of reducing (PASI, skin thickness, spleen index) and a significant reduction in gene expression. In an IMQ-induced psoriasis-like inflammation in mice model, it has been discovered that paquinimod can lower cytokine production and suppress inflammation. Nonetheless, these new findings provide a positive outlook for paquinimod’s therapeutic application in this first stage. All the findings indicated the strong ameliorative effect of paquinimod and it is a promising intervention for psoriasis treatment in future, which may explain its anti-inflammatory activity.
Author Contributions: Raghad Abdulsalam Khaleel,Munaf Hashim Zalzala Conceptualization of and designed the experiments. Raghad Abdulsalam Khaleel performed the experiments and analyzed the data. Yasir Wael Rashid examined the mice and determined PASI score, Munaf Hashim Zalzala revised the paper. Raghad Abdulsalam Khaleel wrote the paper. All of the authors discussed the results and improved the final text of the paper.
Funding: «This research received no external funding»
Institutional Review Board Statement: «The study was conducted according to the guidelines of the Declaration of Baghdad, and approved by the Institutional Review Board (or Ethics Committee) of University of Baghdad College of Pharmacy (12/2020).
Informed Consent Statement: «Informed consent was obtained from all subjects involved in the study.»
Acknowledgement
The data in this article was taken from a Ph.D. thesis submitted to the University of Baghdad’s College of Pharmacy’s Department of Pharmacology and Toxicology. The authors are grateful to the College of Pharmacy at the University of Baghdad for their help.
The data in this article was taken from a Ph.D. thesis submitted to the University of Baghdad’s College of Pharmacy’s Department of Pharmacology and Toxicology. The authors are grateful to the College of Pharmacy at the University of Baghdad for their help.
REFERENCES
1. Alhammad IM, Aseri AM, Alqahtani SAM, Alshaebi MF, Alqahtani SA, Alzahrani RA, et al. A review on updates in management and Treatment of Psoriasis. Arch Pharm Pract. 2021;12(1):74–8.
2. Sahi FM, Masood A, Danawar NA, Mekaiel A, Malik BH. Association between Psoriasis and Depression: A Traditional Review. Cureus. 2020;12(8):8–13.
3. Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20(6):1–28.
4. Chowdhury S, Chakraborty P Pratim. Universal health coverage ‑ There is more to it than meets the eye. J Fam Med Prim Care [Internet]. 2017;6(2):169–70.
5. Ueyama A, Yamamoto M, Tsujii K, Furue Y, Imura C, Shichijo M et al. Mechanism of the pathogenesis of imiquimod-induced skin inflammation in the mouse: A role for interferon-alpha in dendritic cell activation by imiquimod. J Dermatol. 2014;41(2):135–43.
6. Schelbergen RF, Blom AB, Leanderson T, Eriksson H, van den Berg WB, van der Kraan PM, et al. The S100A9 inhibitor paquinimod (ABR-215757) reduces synovial activation, osteophyte formation, and cartilage damage in experimental osteoarthritis. Osteoarthr Cartil. 2014;22(2014): S482–3.
7. Lee JU, Park JS, Jun JA, Kim MK, Chang HS, Baek DG, et al. Erratum: inhibitory Effect of Paquinimod on a Murine Model of Neutrophilic Asthma Induced by Ovalbumin with Complete Freund’s Adjuvant (Canadian Respiratory Journal (2021) 2021:9 (8896108).
8. Pettersson NF, Deronic A, Nilsson J, Hannibal TD, Hansen L, Schmidt-Christensen A, et al. The immunomodulatory quinoline-3-carboxamide paquinimod reverses established fibrosis in a novel mouse model for liver fibrosis. PLoS One. 2018;13(9):1–14.
9. Draibe J, Pepper RJ, Salama AD. Treatment with quinoline-3-carboxamide does not successfully prevent immune-mediated glomerulonephritis in mice. Nefrologia [Internet]. 2016;36(6):687–93.
10. Zhang S, Liu X, Mei L, Wang H, Fang F. Epigallocatechin-3-gallate (EGCG) inhibits imiquimod-induced psoriasis-like inflammation in BALB / c mice. BMC Complement Altern Med. 2016;16(1):1–11.
11. Nakajima K, Kanda T, Takaishi M, Shiga T, Miyoshi K, Nakajima H, et al. Distinct Roles of IL-23 and IL-17 in the Development of Psoriasis-Like Lesions in a Mouse Model. J Immunol. 2011;186(7):4481–9.
12. Coo Luna LG. Preparation of tissue. Man Histol. 1968;(April):1–36.
13. Luna LG. Preparation of tissue. Man Histol. 1968;(April):1–36.
14. Atawodi SE, Atawodi JC, Dzikwi AA. Polymerase chain reaction: Theory, practice, and application: A review. Sahel Medical Journal. 2011; 13.
15. Hobi, A. A. .; AL-Helal, A. . Effect Of Alcoholic Extract Of Opuntia Ficus Indica On Semen Quality Of Awassi Rams After Different Cooling Periods. ). Journal of Life Science and Applied Research. 2021, 2, 9-13.
16. Grine L, et al. An inflammatory triangle in psoriasis: TNF, type I IFN, and IL-17. Cytokine Growth Factor Rev (2014).
17. Stenström M, Nyhlén HC, Törngren M, Liberg D, Sparre B, Tuvesson H, et al. Paquinimod reduces skin fibrosis in tight skin 1 mice, an experimental model of systemic sclerosis. J Dermatol Sci. 2016;83(1):52–9.
18. Levine, Danielle Gottlieb, Alice. Evaluation and Management of Psoriasis: An Internist’s Guide.Medical Clinics of North America.2009:93(6)1291-1303.
19. Najim, Y. S., Mohammed, Th. T. & Al-Khalani, F. M. H. The effect of the use of different levels of Azolla to male broilers diets in the production and physiological performance and economic feasibility. Biochemical and Cellular Archives. 2020, 20(1): 573-580. Doi: 10.35124/bca.2020.20.1.573.
20. Abdulridha SH, Kadhim DJ, Abdul Razzak SA. Assessment of quality of life in a sample of Iraqi patients with psoriasis. Iraqi J Pharm Sci. 2020; 29. (2): 161–8.
Received: January 15, 2023 / Accepted: February 25, 2023 / Published:15 March 2023
Citation. Khaleel R A, Zalzala M H, Rashid Y W. Immune-protective effect of topical paquinimod administration against imiquimod-induced psoriasis-like inflammation in mice.Revis Bionatura 2023;8 (1) 90 http://dx.doi.org/10.21931/RB/2023.08.01.90




















