Vol 8 No 1 2023 – 59

COVID-19 vaccine causes of acceptance and rejection among university students in Baghdad
1 Ministry of Health, Alrusafa directorate, Baghdad, Iraq; salmanshaymaa@gmail.com,
2 Al-Rasheed University College; vsdasd9@gmail.com,
3 Ministry of Health, Alrusafa directorate, Baghdad, Iraq; dr_samaa32@yahoo.com,
*Corresponding author. vsdasd9@gmail.com
Available from: http://dx.doi.org/10.21931/RB/2023.08.01.59
ABSTRACT
Despite numerous recommendations concerning individual and social preventive measures, including quarantine, wearing a mask, physical distancing, and handwashing, vaccination with effective and safe vaccines is still the most effective measure to break the chain of coronavirus SARS-Co2 transmission; still, vaccine hesitancy is a significant barrier to achieve high vaccination coverage against infectious diseases.
An observational cross-sectional study was conducted among students of different universities (medical and non-medical) in Baghdad city Iraq using an online structured google form questionnaire from October 20 to November 20, 2021, and a final number of 658 students were included in the study. Causes of acceptance and rejection of the coronavirus vaccine were tested through the questionnaire.
Of the total 658 participants, 557(84.7%) had received the vaccine before the start of the study and only 101 (15.3%) were not vaccinated; of them, more than half , 58(57.4%) were willing to, and the remaining 43(42.6%) refused to receive COVID-19 vaccination. Accordingly, the acceptance rate of the vaccine among the total participants was 93.5%, and the rejection rate was only 6.5%.
The most chosen cause of vaccine acceptance was that they believed the vaccine protected them, their families and the community against COVID-19 infection and its complications with 63.5%. The most chosen rejection cause was fear of side effects of the vaccine, with 62% of the rejecting participants, followed by 28% having doubts about the vaccine’s efficiency in protecting against COVID-19 infection.
In this study, although the majority of the participants were willing to be vaccinated, still around one-third of them were under pressure from the government obligations and did not accept the vaccine due to their own convictions; education programs should be designed and directed to remove barriers to negative vaccine beliefs and perception to increase the vaccine coverage in the community.
Keywords: COVID-19 vaccination, university students, vaccine acceptance, vaccine rejection.
INTRODUCTION
Globally, the coronavirus disease 2019 (COVID-19) caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused illness and death in different populations more than any other pandemic in the last hundred years. As of October 22, 2021, nearly 242 million people had been infected, while 4.9 million had died worldwide1.
The pandemic of COVID‐19 is considered a global challenge for all countries worldwide to contain its spread. Efforts and campaigns for prevention, early diagnosis, and medical management are being led by the World Health Organization (WHO) and numerous research teams and clinical experts worldwide. There are nonspecific antiviral medications for COVID‐19, and among the used drugs, few showed success in reducing mortality among patients with COVID‐19; in addition, compliance of humans with social distancing and using face masks for prevention is unguaranteed. Thus, the best strategy to control and gradually silence this pandemic is to develop an effective vaccine2.
In December 2020, several vaccines were authorized to prevent COVID-19 infection , and although vaccines have been a successful measure of disease prevention for decades, however, vaccine hesitancy and refusal are significant concerns globally, prompting the World Health Organization (WHO) to declare this uncertainty among the top 10 health threats in 20193.
World Health Organization defines vaccine hesitancy as a «delay in accepting or refusing safe vaccines despite availability of vaccine services.» It is caused by complex and different specific factors that vary across time, place, and other vaccines and is influenced by issues such as complacency, convenience, confidence, and sociodemographic contexts. Vaccine hesitancy could be related to misinformation and wrong theories often spread online, including social media4.
As mentioned above, vaccines are one of the most effective tools for protecting people against COVID-19. It is not uncommon for governments and institutions to mandate specific actions or types of behavior to protect the wellbeing of individuals or communities and overcome vaccine refusal. Such policies can be ethically justified, as they may be crucial to protecting the health and wellbeing of the public; still, critical ethical considerations and caveats should be explicitly evaluated and discussed by governments and/or institutional policy-makers who may be considering mandates for COVID-19 vaccination5.
In Iraq, significant transmission and the rise in case numbers put enormous pressure on hospitals, intensive care units, and health workers. While preventive measures can effectively reduce virus transmission, their effectiveness depends on strict application by all citizens. The vaccines arrived in March 2021, accompanied by the launch of a nationwide vaccination campaign that hoped to be a game-changer in the battle against COVID-19.
In Iraq, as in other countries worldwide, hesitancy and refusal of COVID-19 vaccination is challenging as the acceptance rate in most Arab countries is not high 6. For this reason, this study aims to explore the level of COVID‐19 vaccine acceptance and refusal among university students and determine the factors and barriers that may affect vaccination decision‐making among them since they are considered an important target group for vaccination now as the study returned from online to actual in-school study this year.
MATERIALS AND METHODS
Study Design and Setting
An observational cross-sectional study was conducted among students of different universities (medical and non-medical) in Baghdad city Iraq using an online structured google form questionnaire from October 20 to November 20, 2021; a total number of 693 participants answered the questionnaire of those 35 answers were discarded as they did not meet the research credibility and the remaining 658 were included in the study. We have used Gmail as the main way of contact with participants after an initial announcement about the study in the social groups of medical students in Baghdad universities.
The questionnaire
The researchers designed and developed the questionnaire after literature reviews 7-9. The questionnaire was developed in English and then translated into Arabic, the primary language in Iraq. A panel of experts confirmed the content validity of the questionnaire. It was designed using google Forms and distributed online to the students.
The questionnaire consisted of three main parts; the first included the sociodemographic characteristics of the participants, whether they received the COVID-19 vaccine or not; the second part had the causes of acceptance to receive the vaccine, which should be answered by those who received or willing to receive the vaccine soon or in the future. In contrast, the third part contains the causes of refusal of the vaccine, which should be answered by those who rejected the vaccine. All of the questions were assigned to be mandatory responses to items to avoid incompleteness and missing data.
Ethical consideration
Research ethical approval and permission from Baghdad Al-Rusafa health directorate for collection of data and performance of the study and permission was taken from all the participants with confidentiality and privacy of data were guaranteed during the study, the collected personal information was stored in secure folders that could only be accessed by the researchers and protected from any unauthorized access. The privacy and confidentiality and how to be guaranteed were explained to all participants.
Data Analysis
All data were collected into the Excel sheet and statistically analyzed using SPSS software version 26; simple descriptive analyses, including frequencies and percentages, were computed for demographic characteristics, and the chi-square test was used to find associations between sociodemographic factors and the acceptance or rejection of the participants to the vaccine, a P value of equal or less than 0.05 is considered significant
RESULTS
The study included 658 students from different universities in Baghdad; of those, 367 (55.8%) were medical students (including medicine, dentistry and pharmacy) and 291 (44.2%) were non-medical students, 374(56.8%) were female, 284 (43.2%) were male.
Age was not a parameter in our study since all the participants were in the same age group (18-24 years).
622(94.9%) of the participants were unmarried, 32 (4.9%) were married, and only 4 (0.6%) were divorced or widows; regarding chronic diseases, the majority, 594 (90.3%), had no chronic diseases (table1).
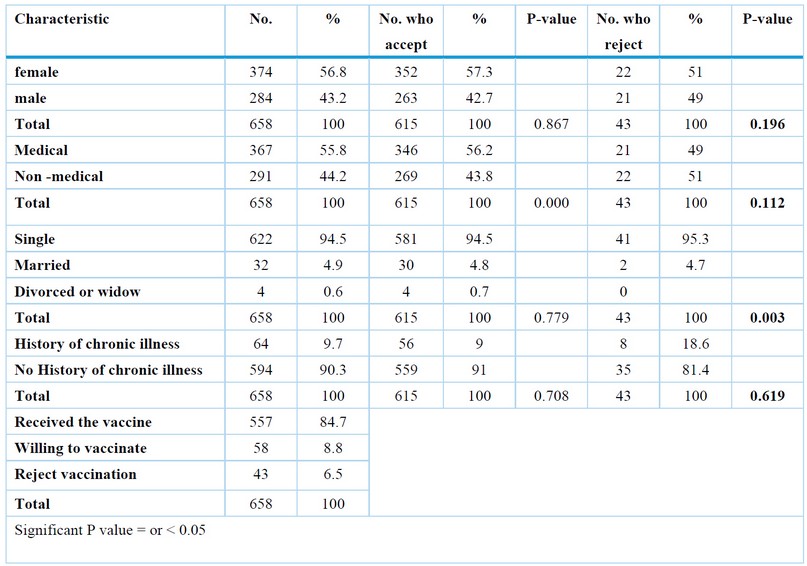
Table1. Sociodemographic characteristics and their effect and association with acceptance and rejection of COVID-19 vaccine
Of the participants, 557(84.7%) had received the vaccine before the start of the study , and only 101 (15.3%) were not vaccinated; of them, more than half, 58(57.4%), were willing to, and the remaining 43(42.6%) refused to receive COVID-19 vaccination. Accordingly, the acceptance rate of the vaccine among the total participants was 93.5%, and the rejection rate was only 6.5% (Table 1).
Of those who received or were willing to receive the vaccine and were allowed to choose more than one cause, 63.5% accepted to receive the vaccine because they believed that it protected them, their families and the community against COVID-19 infection and its complications. In contrast, 37% accepted the vaccine because of the obligation put by the government and the university to attend classes and continue their study, and 47.6% mentioned that the cause of acceptance was the pressure of their families to receive the vaccine, which may reflect the belief of these families in the effectiveness of the vaccine in the protection of their sons and daughters from infection (table 2).

Table 2. Causes of acceptance of the COVID -19 vaccine among the participants who accept the vaccine
Regarding the causes of rejection of the vaccine, again, the participants who rejected the vaccine were allowed to choose more than one cause, and the most frequently selected reason was that they were afraid of the side effects of the vaccine, with 62% of the rejecting participant, followed by 28% had doubts in the efficiency of the vaccine in protection against COVID-19 infection, then 18.6% reject the vaccine as their families refused it. At the same time, 14.7% and another 14% rejected the vaccine because they feared its effect on their chronic diseases and due to the information found in social media against the vaccine, respectively.
None of the participants who rejected the vaccine chose each of the two causes, which are not believing in the existence of COVID-19 infection and taking the vaccine can lead to the spread of the disease to others (table 3).

Table 3. Causes of rejection of the COVID-19 vaccine among those who reject the vaccine
We tried to find if there is any association between the sociodemographic characteristics and the acceptance or rejection of the vaccine; in a total of 615 who accepted the vaccine, the females had a higher acceptance rate (57.3%) compared to receiving males (42.7%), but no statistical significance found.
There was a statistically significant association between the type of study and accepting the vaccine as those with medical studies 55.8% received the vaccine compared to those of non-medical studies with only 44.2%.
As the vast majority of the participant students were not married (94.5%) so, the majority of those who accepted the vaccine was also not married (94.5%) among the total vaccine acceptant, but what is noted is that all those divorced or widows accepted the vaccine, but since they represent only 0.7% of the total participants, again they constituted a small portion of those who accept the vaccine (0.6%).
The same thing applied to those with no chronic disease as they represent 90.3% of the total participants, so 91% of those who accepted the vaccine had no chronic diseases, but again statistically significant association was not found (Table 1).
Regarding rejection of the vaccine in a total of 43 rejecting participants, the only statistically significant association was found with marital status as a higher rejection rate (95.3%) in the non-married compared to (4.7%) in those who were married.
Those with no chronic illness rejected the vaccine (81.4%) more than those with chronic diseases (18.6%), but no great effect of the sex or type of study was found on the rejection of the vaccine (Table 1).
DISCUSSION
Vaccination coverage is highly influenced by its acceptability, while vaccine hesitancy is a barrier to achieving high vaccination coverage against infectious diseases. Therefore, understanding its determinants is necessary to aid acceptability and tackle vaccine hesitancy, and this is applied to the COVID-19 vaccine10.
Our study was conducted on university students since they are an essential knowledgeable part of the community to assess their acceptance and rejection of the COVID-19 vaccine and the factors affecting their will regarding receiving it.
The study showed a high acceptance rate among participants of 93.5% compared to 56.3% in a study on university students in the United Arab Emirates11 and only 37.3% of medical students in Uganda12 and 34.9% of Egyptian medical students2.
This high acceptance was in the majority (63.5%) due to the belief of the importance of the vaccine in protection against the COVID-19 infection, and 47.6% accept the vaccine under the will and pressure of their families which may also reflect the belief of the parents in the importance of the vaccine in the protection of their sons and daughters, this in the collection reveals that education, positive attitude and beliefs are related to higher willingness to vaccination and higher coverage rate which is found in a study on medical students in Europe13.
In addition, 37% accept the vaccine due to the obligations and rules put by the government and the university; this factor also causes a higher acceptance score among students in a study done in South Carolina14.
Although the rejection rate was low (6.5%) we tried to find the factors that caused this decision, here the fear of side effects of the vaccine was the most chosen factor (62%); the same finding was found in a Turkish study on nursing students15 and a study among Malaysians7 and Bangladesh16 where this was the most causative factor for hesitancy and refused of the vaccine. Although primarily non-serious, side effects can make vaccination a disagreeable experience and side effect concerns are among the most common causes of vaccine hesitancy; for example, a recent US poll found 90% of COVID-19 vaccination refusers were more worried about vaccine side effects than COVID-19 infection itself which may be related to psychological factors17.
The next commonest cause (28%) of rejection was that they believed the vaccine was not effective in protecting them against the infection same as in the Malaysian study (8) and the same in a study in Saudi Arabia which showed the majority of refusers may accept the vaccine if additional studies confirmed safety and effectiveness18.
14% of rejecting students mentioned that they rejected the vaccine due to the effect of information on social media; this reflected the negative effect of the misinformation found on social media on the acceptance of vaccination, as in the study done in the United Kingdom and the United States which showed that scientific-sounding misinformation is more strongly associated with declines in COVID-19 vaccination intent19.
It is noted that no one of the rejecters chose the causes that they do not believe in the existence of COVID-19 infection. If they receive the vaccine, they may spread the virus to others, which are wrong belief found around the population, but our study group (university students) found it to be away from these beliefs.
Regarding sociodemographic characteristics, the female students had a higher acceptance rate which is the same as the study on Czech university students20.
A statistically significant association was found regarding the type of study with acceptance of the vaccine as the medical had a higher acceptance rate (55.8%) compared to non-medical students (44.2%); the same finding was found in a study done in Pakistan as medical students were more willing to get vaccinated, largely owing to their knowledge and understanding of vaccines21, this explanation could be applied to our study, in addition to their increased risk of exposure during their study courses in the hospitals and medical centers that make them willing to be vaccinated.
Students with no chronic diseases had a higher acceptance rate compared to those with chronic diseases since there is only 9.7% of the total participant had chronic diseases, but we found that of a total of 64 students with chronic diseases, the acceptance rate was 87.5% which is still lowest than 94% found in the remaining 594 students without chronic conditions; also this could be related to fear from the effect of the vaccine on the chronic diseases which contributed to 14% of the causes of vaccine rejection in this study.
There is a statistically significant association between marital status and rejection of the vaccine, where the non-married had a higher rejection rate among those who rejected the vaccine (95.3%), and this could be related to the small percentage of the married students (4.9%) compared to 94.5% of non-married among the total participants. This is contrary to a study done in China, where vaccine rejection was higher among the married population22.
At the time of the start of this research, we directed our study to the university students since they were targeted to be vaccinated by the government as their study returned from the remote online to the regular university in presence lectures, which necessitated their protection against COVID-19 infection by vaccination.
CONCLUSIONS
The majority of the participants were willing to be vaccinated, still around one-third of them were under pressure the government obligations and did not accept the vaccine due to their conviction; others accepted the vaccine due to the will of their families , which reflects that although there is a pandemic and the best way to protect themselves and others is vaccination, still, there is some degree of hesitation even in the educated groups as the university students in our study. As we tried to find the most important causes of vaccine rejection, which were fear of the side effects of the vaccine and doubt about the efficiency of the vaccine, so, the COVID-19 pandemic immunization and education programs should be designed and directed to remove barriers to negative vaccine beliefs and perception to increase the vaccine coverage in the community. Further studies are needed on other and broader groups of the Iraqi population and focus on the effect of vaccine education and an attempt to change attitudes and beliefs on vaccine acceptance. The rules and legislations put by the government by making the COVID-19 vaccination a must for entering college classes and public places play an important role in increasing vaccine coverage.
Author Contributions: Conceptualization, Shayma Ali.; methodology, Israa Ali.; software, Raid Hashim; validation, Raid Hashim, Shayma Ali and Israa Ali; formal analysis, Shayma Ali and Israa Ali; investigation, Raid Hashim; resources, Israa Ali; data curation, Shayma Ali; writing—original draft preparation, Shayma Ali; writing—review and editing, Raid Hashim; visualization, Raid Hashim; supervision, Israa Ali; project administration, Shayma Ali; funding acquisition, Israa Ali.
Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted following the Declaration of Helsinki and approved by the Ethics Committee of the Iraqi ministry of health.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Written informed consent has been obtained from the participants to publish this paper.
Data Availability Statement: Not applicable
Conflicts of Interest: The authors declare no conflict of interest
REFERENCES
1. Muhajarine N, Adeyinka DA, McCutcheon J, Green KL, Fahlman M, Kallio N. COVID-19 vaccine hesitancy and refusal and associated factors in an adult population in Saskatchewan, Canada: Evidence from predictive modelling. PLOS ONE. 2021;16(11):e0259513.
2. Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. 2021;93(7):4280-91.
3. Al-Qerem WA, Jarab AS. COVID-19 Vaccination Acceptance and Its Associated Factors Among a Middle Eastern Population. Frontiers in Public Health. 2021;9.
4. Razai MS, Chaudhry UAR, Doerholt K, Bauld L, Majeed A. Covid-19 vaccination hesitancy. BMJ. 2021;373:n1138.
5. World Health O. COVID-19 and mandatory vaccination: ethical considerations and caveats: policy brief, April 13 2021. Geneva: World Health Organization; 2021 2021. Contract No.: WHO/2019-nCoV/Policy_brief/Mandatory_vaccination/2021.1.
6. Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Global Health Research and Policy. 2021;6(1):23.
7. Syed Alwi SAR, Rafidah E, Zurraini A, Juslina O, Brohi IB, Lukas S. A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health. 2021;21(1):1129.
8. Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLOS ONE. 2021;16(8):e0256110.
9. Mant M, Aslemand A, Prine A, Jaagumägi Holland A. University students’ perspectives, planned uptake, and hesitancy regarding the COVID-19 vaccine: A multi-methods study. PLOS ONE. 2021;16(8):e0255447.
10. Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, et al. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines. 2021;9(3):300.
11. Shahwan M, Suliman A, Abdulrahman Jairoun A, Alkhoujah S, Al-Hemyari SS, Al-Tamimi SK, et al. Prevalence, Knowledge and Potential Determinants of COVID-19 Vaccine Acceptability Among University Students in the United Arab Emirates: Findings and Implications. J Multidiscip Healthc. 2022;15:81-92.
12. Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical Medicine and Health. 2021;49(1).
13. Kaya MO, Yakar B, Pamukçu E, Önalan E, Akkoç RF, Pi̇ri̇nçci̇ E, et al. Acceptability of a COVID-19 vaccine and role of knowledge, attitudes and beliefs on vaccination willingness among medical students. The European Research Journal. 2021;7(4):417-24.
14. Tam CC, Qiao S, Li X. Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Psychology, Health & Medicine. 2022;27(1):150-61.
15. Yeşiltepe A, Aslan S, Bulbuloglu S. Investigation of perceived fear of COVID-19 and vaccine hesitancy in nursing students. Human Vaccines & Immunotherapeutics. 2021;17(12):5030-7.
16. Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MZ, Sultana R, et al. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the health belief model and the theory of planned behavior model. Vaccines. 2021;9(12):1393.
17. Geers AL, Clemens KS, Faasse K, Colagiuri B, Webster R, Vase L, et al. Psychosocial Factors Predict COVID-19 Vaccine Side Effects. Psychotherapy and Psychosomatics. 2021:1.
18. Magadmi RM, Kamel FO. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021;21(1):1-8.
19. Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature human behaviour. 2021;5(3):337-48.
20. Riad A, Pokorná A, Antalová N, Krobot M, Zviadadze N, Serdiuk I, et al. Prevalence and drivers of COVID-19 vaccine hesitancy among Czech university students: National cross-sectional study. Vaccines. 2021;9(9):948.
21. Sadaqat W, Habib S, Tauseef A, Akhtar S, Hayat M, Shujaat SA, et al. Determination of COVID-19 vaccine hesitancy among university students. Cureus. 2021;13(8).
22. Dong C, Liang Q, Ji T, Gu J, Feng J, Shuai M, et al. Determinants of Vaccine Acceptance against COVID-19 in China: Perspectives on Knowledge and DrVac-COVID19S Scale. International journal of environmental research and public health. 2021;18(21):11192.
Received: January 15, 2023 / Accepted: February 25, 2023 / Published:15 March 2023
Citation: Ali S, Hashim R, Ali I. COVID-19 vaccine causes of acceptance and rejection among university students in Baghdad. Revis Bionatura 2023;8 (1) 59. http://dx.doi.org/10.21931/RB/2023.08.01.59




















