Vol 8 No 1 2023 – 37

1.Department of Biology, College of Science, Misan University, Maysan 62001, Iraq.
*Correspondence author Email: raedsaddam@uomisan.edu.iq
Available from: http://dx.doi.org/10.21931/RB/2023.08.01.37
ABSTRACT
The current study was designed to examine the association between breast cancer grading and levels of CA15-3 was studied in addition to the correlation between ABO blood groups and breast cancer. The study involved (140) breast cancer women, and (140) blood samples were collected from healthy women who served as control. The total patients were divided according to their ages into three groups (30-39), (40-49) and (≥50), and ABO blood groups. Moreover, the grades of breast cancer were divided into three groups, and their correlation with serum CA15-3 levels was studied. The current study shows a significant correlation between breast cancer grading and levels of serum CA15-3 antigen. The study also showed that breast cancer is elevated with age. The results demonstrated a great association between the ABO blood groups and breast cancer. Blood group type (A) recorded the highest frequency and percentage (42.14%) of patients with breast cancer. The non-A-blood type (O, B and AB) percentage was as follows (32.14%, 19.29% and 6.43%, respectively). Thus, monitoring breast cancer occurrences in women with blood group A early could be an and excellent strategy to control and facilitate the event of breast cancer.
Keywords: Breast cancer, CA15-3, blood groups, breast cancer grading.
INTRODUCTION
Breast cancer is one of the most common cancers and the second most commonest that causes cancer death in women. It is well known that breast cancer initiates in breast tissue, which consists of lobules for milk production and ducts that link the lobules to the nipple 1. Breast cancer can penetrate the duct or gland walls to infiltrate the surrounding fatty tissue of the breast and eventually invade other parts of a woman’s body 1. Many risk factors have been identified to be correlated with breast cancer occurrence, such as family history, obesity, age, diet and environment 2. It has been shown that breast cancer has a strong association with age and that the occurrence of breast cancer was increased in the age group >45 2.
Different approaches exist to detect and monitor breast cancer incidence and progression. For instance, a breast cancer diagnosis can be seen using blood tumor markers, such as cancer antigen CA15-3 or genetic profiles. CA15-3 has been found to be promising for breast cancer diagnosis 3,4.
ABO blood antigens are carbohydrates that are encoded by one gene with three alleles. These antigens are expressed on the erythrocytes surface 2. Based on the presence or absence of erythrocyte surface antigens, ABO blood types are classified into four phenotypes: A, B, AB and O 5. It has been shown that ABO blood type is associated with several diseases such as Hepatitis-B 6, vascular diseases 7, stomach and duodenal ulcer 8, cancer 9 and diabetes mellitus types2 10. Moreover, ABO blood type has also been documented to be associated with cancer occurrence, such as pancreatic cancer 11-13. Indeed, antigens of blood types have been found to have an essential role in various conditions such as cell signaling, cell adhesion, tumorigenesis and metastasis 14. Previous studies have shown that A antigen has similar properties to antigens, A like-antigens, expressed by tumor cells 15. This could explain why people with A blood type are more susceptible to cancer. This study is aimed to study the association between serum CA15-3 antigen and further confirm the potential connection between blood groups and breast cancer in women.
MATERIALS AND METHODS
Sample collection and study design
The present study was implemented in Maysan province/south of Iraq[R1] . The authorization approval for this study was obtained from Maysan Health Department.
The study included 140 breast cancer patients who attended the AL-Shefaa oncology center in Maysan. The specialist medical staff diagnosed breast cancer according to clinical examinations, evaluations of levels of serum cancer antigen 15-3 (CA15-3), and breast biopsy. Moreover, (140) blood samples were harvested from healthy women and served as control.
CA15-3 measurement
The levels of CA15-3 were measured in the serum of patients and the control group using a commercial kit (EIA-3941, DRG, Germany) and based on the manufacturer’s instructions.
Histological examination
A breast biopsy was performed in suspected women with breast cancer for further diagnosis confirmation. Tissue samples were fixed in formaldehyde phosphate buffer[R2] (4%). After dehydration and paraffin embedding, samples were stained (H&E) and examined under light microscopy. The grade of breast cancer was evaluated by using a standard protocol 16.
Identification of ABO blood groups:
The conventional slide agglutination method was used to determine blood group phenotypes (A, B, AB, and O) and according to agglutination reactions that were carried out between blood group specific anti-sera and blood group antigens on the cell,
Statistical analysis
Statistical analysis was carried out using Chi-square and T-tests that were analyzed by SigmaStat program 10.0. Data are introduced as mean values ± standard error of the mean. Statistical significance between the groups was presented as P < 0.05.
RESULTS
Age distribution
The number of patients was exceptionally high in the age group (≥50) years in percent (44.16%), followed by the age group (40-49) years (35%) and then (20.84%) in the age group (30-39) as summarized in table (1).

Table 1. Age distribution of patients and controls.
Levels of CA15-3 antigen in breast cancer and control
CA15-3 antigen has been using commonly as an indicator for breast cancer diagnosis 17. In this study, breast cancer diagnosis of 140 patients and control wasidentified based on serum CA15-3 antigen (Figure1). The results showed a significant augmentation in the levels of serum CA15-3 antigen in patient group as compared with healthy group (Figure1).

Figure 1. Levels of serum CA15-3 measurements. The black box represents patients with breast cancer. Grey box represents control groups. Data represent means ± SEM. #P <0.05 versus control.
CA15-3 levels and breast cancer grading
Diagnosis of breast cancer was also confirmed by using another approach, which was histopathological examinations. It was found that tissue architectures and uniform cells in the grade 1 tissues sample are similar to the normal breast tissue (Figure 3). However, tissue architectures and cells in grades 2 and 3 had different features than normal cells. For instance, histological changes in grade 2 show a moderate variability in tissue architecture, cell size, and shape. In addition, histological examinations of grade 3 showed great destruction in tissue architecture and an apparent variation in cell shape and size (Figure 3). Moreover, this study examined the correlation between the CA15-3 antigen and breast cancer grading. The results found an association between serum CA15-3 antigen levels and the grades of breast cancer (Figure 2), which indicated that serum CA15-3 antigen could be used as an indicator even for early diagnosis.

Figure 2. The percentage of CA15-3 antigen and breast cancer grading. Blue line represents grade 1. Red line represents grade 2. Green line represents grade 3. Data described as percentage; comparisons between groups were done using Chi-square test. P-value £ 0.05 used as a significant levels between the groups.

Table 2. Association between CA15-3 and breast cancer grading .
Distribution of ABO blood groups in patients and controls
The overall distribution ratio of blood groups (A, O, B and AB) of 140 patients was (42.14%, 32.14%, 19.29%, and 6.43%) corresponding to blood groups A, O, B and AB, respectively. In contrast, the distribution ratio of blood groups in control subjects was (28.57%, 25%, 39.29% and 7.14% ) corresponding to groups A, O, B, and AB, respectively. These findings revealed that blood group A has a significant connection with the occurrence of breast cancer compared to the other blood groups, table (3-3 and 4).

Table 3. Blood group distribution of patients and controls.

The Chi^2 value is 32.502. The p-value is < .00001. The result is significant at p < .05.
Table 4. Statistical differences between ABO blood groups in breast cancer patients using the Chi^2 test.
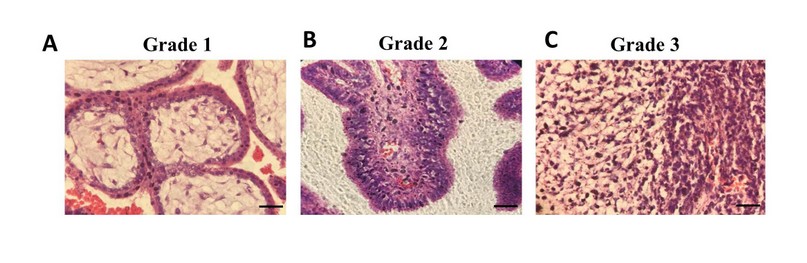
Figure 3. Grades of breast cancer. Hematoxylin & eosin sections from breast tissue of women who had breast cancer. Scale bar = 50 μm. A) grade 1, B) grade 2, C) grade 3.

Figure 4. Blood groups distribution of patients and controls. Percentage of ABO blood groups in controls (Blue line) and patients (Red line).
DISCUSSION
Serum CA15-3 antigen has increased significantly in patients with breast cancer 18. The findings found that serum CA15-3 antigen levels are associated with breast cancer grades (Figure 2). Moreover, A blood type has been shown to have a great connection with breast cancer incidence compared to non-A blood types. Therefore, serum CA15-3 antigen could be a useful independent indicator in breast cancer patients. In addition, these findings indicate that monitoring the occurrence of breast cancer in women with A blood type, especially in young women, could be a valuable strategy to control breast cancer occurrence.
It is well established that CA15-3 antigen has been used as a marker for different types of cancer. Moreover, CA15-3 antigen has been identified to express breast cancer cells [R4] at higher levels than the standard 17. The present study found that serum CA15-3 antigen levels increased significantly in the patient’s group compared to the healthy group (Figure 1). Moreover, the current findings explored the correlation between serum CA15-3 antigen and breast cancer grading. It was found that serum CA15-3 antigen has a significant correlation with the grades of breast cancer[R5] (Table 2). The findings agree with the previous study by Hashim, Z. M et al. 17. The current results could confirm that identifying serum CA15-3 antigen could be a practical diagnostic approach for early breast cancer diagnosis.
It is well known that cancer can occur at any age; however, many cancer types become common after humans get older. It has been shown that breast cancer incidence has a strong association with age 19. The present study revealed that patients with breast cancer fall in the age group ≥50 years (Table 1), which gives a clear idea that age is more likely to be associated with breast cancer incidence. In line with that, a previous study has shown that breast cancer incidence increases with age 20. Moreover, El- Zaemey et al., 2012, have found that breast cancer has a high incidence at age 50 years 21. It has also been shown that age might be one of the risks of breast cancer occurrence and could be increased at age (60) years or even older 22. It is assumed that the reason beyond this might be an increase in the point mutation in the genetic material of DNA, which causes abnormal changes in the chromosome of the cell. Furthermore, it has shown that breast cancer occurrence rates did not elevate in women under age (40). Still, Ductal Carcinoma «in situ» (DCIS) augmented in women of all ages during the same period 21. Another explanation is that estrogen levels would be higher in women who start menstruation early and reach menopause at a late age compared to those with a late menarche or early menopause 23. Moreover, another risk associated with breast cancer development is the age at first pregnancy. For example, the risk of breast cancer is suspected to be reduced in the first full-term pregnancy at a relatively early age compared to those who never have children or those who have their first child relatively late in life 24.
The ABO types are an essential part of transfusion medicine but have been shown to be associated with various diseases 2. For example, it has been documented that blood group A people are more susceptible to Pseudomonas aeruginosa and smallpox 9. The present study identified that the occurrence of breast cancer was significantly higher in patients with blood group A, compared with non – Groups (O, B, and AB) as shown in (Table 3). These findings were in line with previous studies show that cancer incidences are more suspected to be higher in blood group A people compare to non – A groups (O, B , and AB). For example, it has found that the percentage of cancer occurrence was 64%, 22%, 15%, 28%, 13%, and 11%, of salivary gland, stomach, uterus, ovaries, cervix and colon, which were higher in blood type A people as compared with type O 25. It is believed that in people with non-A blood type who have tumors, their tumors can be with antigens with the same properties as A antigens. Tumors with A-like antigens were shown to be recognized by anti-A antibodies and subsequently attack the tumors [R6] 15. This could explain why people with A blood type is more susceptible to tumorigenesis.
CONCLUSION
the present findings show a strong relation between the levels of CA15-3 antigen and breast cancer grading. Moreover, among ABO types, A blood type has a significant association with the occurrence of breast cancer in women compared to other blood types. Accordingly, A blood type has a high risk of breast cancer, so it could be an excellent strategy to monitor breast cancer incidence in young women with blood group A.
Acknowledgment
I am extremely grateful to Health Department in Maysan for authorization approval of this study. Special thanks go to Maryam Ali for her support in collection of blood samples.
Conflict of interest: The author is declared that there is no conflict of interest in regard of this study.
REFERENCES
1. Sharma, G.N., et al., Various types and management of breast cancer: an overview. J Adv Pharm Technol Res, 2010. 1(2): p. 109-26.
2. Meo, S.A., et al., Association of ABO and Rh blood groups with breast cancer. Saudi J Biol Sci, 2017. 24(7): p. 1609-1613.
3. Ebeling, F.G., et al., Serum CEA and CA 15-3 as prognostic factors in primary breast cancer. Br J Cancer, 2002. 86(8): p. 1217-22.
4. Duffy, M.J., Serum tumor markers in breast cancer: are they of clinical value? Clin Chem, 2006. 52(3): p. 345-51.
5. Dean, L. and National Center for Biotechnology Information (US), Blood groups and red cell antigens. 2005, NCBI,: Bethesda, Md.
6. Siransy, L.K., et al., ABO/Rh Blood Groups and Risk of HIV Infection and Hepatitis B Among Blood Donors of Abidjan, Côte D’ivoire. Eur J Microbiol Immunol (Bp), 2015. 5(3): p. 205-9.
7. Zakai, NA, et al., ABO blood type and stroke risk: the REasons for Geographic And Racial Differences in Stroke Study. J Thromb Haemost, 2014. 12(4): p. 564-70.
8. Tanikawa, C., et al., A genome-wide association study identifies two susceptibility loci for duodenal ulcer in the Japanese population. Nat Genet, 2012. 44(4): p. 430-4, S1-2.
9. Gates, M.A., et al., ABO blood group and incidence of epithelial ovarian cancer. Int J Cancer, 2011. 128(2): p. 482-6.
10. Meo, S.A., et al., Association of ABO and Rh blood groups with type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci, 2016. 20(2): p. 237-42.
11. Wolpin, B.M., et al., ABO blood group and the risk of pancreatic cancer. J Natl Cancer Inst, 2009. 101(6): p. 424-31.
12. Iodice, S., et al., ABO blood group and cancer. Eur J Cancer, 2010. 46(18): p. 3345-50.
13. Wolpin, B.M., et al., Pancreatic cancer risk and ABO blood group alleles: results from the pancreatic cancer cohort consortium. Cancer Res, 2010. 70(3): p. 1015-23.
14. Weisbrod, A.B., et al., Association of type-O blood with neuroendocrine tumors in multiple endocrine neoplasia type 1. J Clin Endocrinol Metab, 2013. 98(1): p. E109-14.
15. Abegaz, S.B., Human ABO Blood Groups and Their Associations with Different Diseases. Biomed Res Int, 2021. 2021: p. 6629060.
16. Rakha, EA, et al., Breast cancer prognostic classification in the molecular era: the role of histological grade. Breast Cancer Res, 2010. 12(4): p. 207.
17. Hashim, Z.M., The significance of CA15-3 in breast cancer patients and its relationship to HER-2 receptor status. Int J Immunopathol Pharmacol, 2014. 27(1): p. 45-51.
18. Shering, S.G., et al., Preoperative CA 15-3 concentrations predict outcome of patients with breast carcinoma. Cancer, 1998. 83(12): p. 2521-7.
19. Winters, S., et al., Breast Cancer Epidemiology, Prevention, and Screening. Prog Mol Biol Transl Sci, 2017. 151: p. 1-32.
20. Anderson, D.E. and MD. Badzioch, risk of familial breast cancer. Cancer, 1985. 56(2): p. 383-7.
21. El-Zaemey, S., et al., Breast cancer among Yemeni women using the National Oncology Centre Registry 2004-2010. Cancer Epidemiol, 2012. 36(3): p. 249-53.
22. Quinn, M.J., C. Martinez-Garcia, and F. Berrino, Variations in survival from breast cancer in Europe by age and country, 1978-1989. EUROCARE Working Group. Eur J Cancer, 1998. 34(14 Spec No): p. 2204-11.
23. Dall, G.V. and K.L. Britt, Estrogen Effects on the Mammary Gland in Early and Late Life and Breast Cancer Risk. Front Oncol, 2017. 7: p. 110.
24. Susan P. Helmrich et al., Risk factors for breast cancer, American Journal of Epdemiology, Volume 117, Issue 1, January 1983, Page 35-45, https://doi.org/10.1093/oxfordjournals.aje.a113513.
25. Garratty, G., Blood groups and disease: a historical perspective. Transfus Med Rev, 2000. 14(4): p. 291-301.
Received: December 23, 2022 / Accepted: January 30, 2023 / Published:15 February 2023
Citation: Madhi R. Diagnostic [R7] and serological study of Breast Cancer in women in Maysan Province, Iraq. evis Bionatura 2023;8 (1)37. http://dx.doi.org/10.21931/RB/2023.08.01.37




















