Vol 3 No 1 2018 – 13
REVISION/REVIEW
Cytokines in the physiopathology of depression
Citoquinas en la fisiopatología de la depresión
María Belén Paredes, María Eugenia Sulen
Available from: http://dx.doi.org/10.21931/RB/2018.03.01.13
ABSTRACT
This paper presents a bibliographical review on the relevance of the possible role of cytokines in depression.There is a consideration of the existing approaches to detection and diagnosis of depression; they are classified according to different criteria such as design methodologies and applications. Although the etiology of depression is still an issue, the focus of this paper is to highlight the various studies regarding the interactions of the immune system and brain activity linked to depression. These interactions are particularly important when trying to find a correlation between proinflammatory cytokines (such as IL-1, IL-6, and TNF-α) and depression. This includes a brief comparison of results obtained by different studies.
Keywords: depression, cytokines, inflammation, TNF-α, IL-1, IL-6
RESUMEN
Este artículo presenta una revisión bibliográfica sobre la relevancia del posible rol de las citoquinas en la depresión. Se tienen en cuenta los enfoques existentes para la detección y el diagnóstico de la depresión, estos han sido clasificados según diferentes criterios, como las metodologías de diseño y las aplicaciones. Aunque la etiología de la depresión sigue siendo un problema, el objetivo de este documento es mostrar los diferentes estudios sobre las interacciones del sistema inmune y la actividad cerebral relacionada con la depresión. Estas interacciones son particularmente importantes cuando se trata de encontrar una correlación entre las citoquinas proinflamatorias (como IL-1, IL-6 y TNF-α) y la depresión. También se incluye una breve comparación de los resultados obtenidos en diferentes estudios.
Palabras clave: depresión, citoquinas, inflamación, TNF- α, IL-1, IL-6
INTRODUCTION
Depression is a mental health disorder characterized by a group of affective, cognitive and somatic symptoms.1Depression boards a broad spectrum of clinical presentations,2 for this reason, depressive disorders are classifiedinto three main subclasses: Major Depressive Disorder, Dysthymic Disorder and Depressive Disorder NOS (NoOtherwise Specified). Each of them is characterized by the presence to greater or lesser degree of different features such as psychotic, catatonic, atypical and chronic.3 The fourth version of the Diagnostic and statistical manual of mental disorders (DSM- IV) is used to diagnose depression,4 and tests like the Hamilton Depression Rating Scale (HDRS) and the Montgomery-Asberg Depression Rating Scale (MADRS) are used in several studies in order to rate depressive symptoms to determine the severity of depression.5,6 Cognitive and sleep disturbances, fatigue, appetite suppression and depressed mood (sickness behaviour) are recognized as the most common symptoms of this disorder.2 However, to determine the etiology and physiopathology of depression is still an issue because of its heterogeneity and the fact that depression appears concomitantly with many other diseases such as diabetes, rheumatoid arthritis and coronary heart disease.2,3,7
Major depressive disorder (MDD), the most severe in the classification of depressive disorders, is considered amajor public health concern with 4% of the adult population presenting active symptoms.8-10 It is associated with social dysfunction, which affects everyday life activities, increased risk of substance abuse, obesity, and suicide.8,11,12 Furthermore, 13 % of people in the USA and 27% of people in Europe have episodes of major depression at least once in their life2. Currently, there are several studies regarding the interactions between the immune system and the brain activity focused on finding a more accurate representation of depression physiopathology. In particular, there is an increased interest in the consequences of inflammation in depressionand the role of proinflammatory cytokines such as IL-1, IL-6, and TNF-α. The consideration of a new approach regarding inflammation is based on the fact that illnesses promoting inflammatory responses are associated withhigher rates of depression, the administration of cytokines induces depressive episodes in non-psychiatric patients, the therapeutic administration of cytokines has led to depression in up to 50% of the patients, and that cytokines induce behaviors that are commonly present as symptoms of depression.13-20
The study aims to review the existing information about the relevance of the possible role of cytokines in depression and the underlying mechanisms.
Cytokines
Cytokines are large polypeptide regulatory mediator proteins secreted by white blood cells and other cells in the body. They play a role in the immune system specifically in inflammatory responses, the regulation of growth, differentiation, and function of cells. The most common classification of cytokines is into families of interleukins, tumor necrosis factors (TNF), interferons (INF), chemokines, haematopoietins and colony stimulating factors (CSF).21
Interleukin-1 (IL-1) is the prototypic proinflammatory cytokine. It appears in two forms: IL-1alpha and IL-1beta. It functions as an immunoadjuvant as it is primarily under immune system control and it is highly inflammatory. The leading producers of IL-1 in the body are monocytes in the blood and macrophages residing in tissues in the body. Many viruses, fungi, bacteria, spirochetes, as well as other infectious agents such as urate, asbestos, silica, numerous cytokines (IL-1, IL-2, TNF, IFNα, IFNβ, IFNγ, macrophage-colony stimulating factor, transforming growth factorβ) among many other chemicals induce IL-1 production. Also, surgery, trauma, tissue damage, malignant cells, organ dysfunction and dying tissue trigger IL-1 release. As we can see, there is no secretion of cytokines unless the immune system is stimulated by either a biological or a psychological danger.3,22
Tumor necrosis factor (TNF) is a broad-spectrum (pleiotropic) cytokine. It has two forms, TNF alpha made by monocytes and macrophages, and TNF beta which is made by lymphocytes.
IL-1 triggers cells to make TNF and TNF induces cells to produce IL-1. When they work together, they have more powerful effects than each one working alone. TNF causes tumor cell necrosis and apoptosis. It has a significantrole regulating morphogenesis, the sleep-wake cycle in lymph node follicle and germinal center formation as well along with host defense against bacterial and viral infection. TNF is a crucial mediator of both acute and chronic systematic inflammatory reactions. It not only induces its secretion, but it also stimulates the production of other inflammatory cytokines and chemokines. TNF has been the center of study for its roles in normal physiology, acute inflammation, chronic inflammation, autoimmune disease and cancer-related inflammation.3,23 TNF-α has been hypothesized as a potential modulator of the serotonin transporter (SERT or 5-HTT), consequently 5-HT uptake, and brain availability.24
Interleukin-6 (IL-6) is a pleiotropic cytokine, which are primary in host defense thanks to its wide range of immune and hematopoietic activities. The production of IL-6 occurs at the site of inflammation. IL-6 also stimulates the production of acute phase proteins in response to varied stimuli. It is involved in many proliferative, differentiative, and maturation processes depending on the nature of the target cell. The overexpression of IL-6 has been related to pathology of countless diseases that include multiple myeloma, rheumatoid arthritis, Castleman’s disease, psoriasis, and post-menopausal osteoporosis.8,25,26
Relationship between serotonin, tryptophan, and cytokines
One of the theories that explain the causes of depressive disorders is the monoamine theory that has been widely used to produce antidepressant drugs to correct the shortage of monoaminergic neurotransmission in patients with this diagnosis. Serotonin or 5-hydroxytryptamine (5-HT) is a monoamine neurotransmitter biochemically derived from the essential amino acid, tryptophan. The action of serotonin is through membrane receptors in both central and peripheral nervous systems as in non-neuronal tissues such as the gastrointestinal and endocrine systems.27Reduced concentrations of serotonin in the synaptic cleft and increase of reuptake by serotonin transporters are described as the main factors that contribute to depression. This is because evidence of alleviation of depressive symptoms using drug treatments that either increase the concentration of serotonin or inhibit its reuptake is available.28 Furthermore, alterations in SERT expression and activity associated with variations in the human SERT gene are linked to mental illness.29 In addition, related to serotonin metabolism, patients with major depression show low plasma levels of tryptophan, which in turn reduces the availability of the precursor for 5-HT synthesis, decreasing the levels of serotonin in the brain.30 Moreover, the inflammatory approach to describe depressive disorders pictures many mechanisms by which proinflammatory cytokines reach the brain and affect monoamine metabolism.29,31
Cytokine signals are able to reach the brain through humoral, neural and cellular pathways. Cytokines are relatively large proteins (ranging from 6–70 kDa) making them unable to pass through the blood-brain barrier (BBB).31 The presumptive non-exclusive mechanisms of how cytokines access the central nervous system (CNS) are: 1.) Direct crossing of cytokines into the CNS, this occurs in the periventricular organs, where the blood-brain barrier (BBB) is physiologically absent, less restrictive (e.g. organum vasculosum laminae terminalis (OVLT) and the median eminence) or when it becomes leaky, the integrity of the BBB may be impaired due to traumas or certain pathological conditions resulting in increased access of various inflammatory cells and molecular constituents, including cytokines, to the brain, 2.) Migration of cytokines by means of paracellular and transmembranous diffusion or active transport via saturable cytokine-specific molecules on brain endothelium, 3.) Activation of endothelial cells, responsible for the subsequent release of second messengers like nitric oxide (NO) and prostaglandins (PGs) within the brain parenchyma, 4.) Transmission of cytokine signals via afferent nerve fibers, such as the vagus nerve, 5.) Entry into the brain parenchyma of peripherally activated monocytes.14,32,33
Cytokines may induce depressive symptoms by down-regulating the synthesis of serotonin. This might be because of the relationship between the immune system and the induction of indoleamine 2,3-dioxygenase (IDO). This enzyme is expressed in the neuroglia such as microglia, astrocytes, and neurons as well as in macrophages and dendritic cells. This enzyme is highly inducible by some cytokines including IFN-γ, TNF-α, IL-1, and IL-6 through activation of a number of inflammatory signal transduction pathways these being signal transducer and activator of transcription 1a (STAT1a), interferon regulatory factor (IRF)-1, NF-kB and p38 MAPK.14,34 IDO switches the metabolism of tryptophan (TRP) toward the synthesis of kynurenine and quinolinic acid, to the detriment of serotonin synthesis (Figure 1). IDO is involved in depression not only because of its effects on serotonin biosynthesis but also because of its putative contributions to excitotoxicity and oxidative stress. 31,35,36IDO’s activity is augmented by the chronic activation of the immune system; this includes coronary heart disease, immunotherapy, obesity, acquired immunodeficiency syndrome (AIDS), atherosclerosis, and rheumatoid arthritis.37
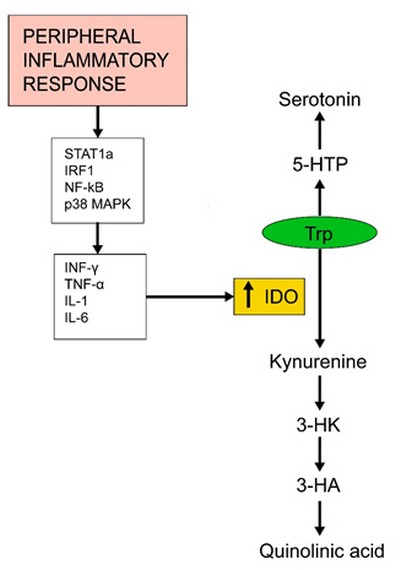
Figure 1. Induction of IDO by cytokines switches the metabolism of tryptophan toward the synthesis of kynurenine and quinolinic acid, to the detriment of serotonin production
Conditions that support the inflammatory hypothesis in the physiopathology of depression
Stress and depression
Stress is common in everyday life; however, traumatic stress can be a relevant factor for CNS illnesses as well as peripheral organ systems.38 Also, chronic stress initiates changes in the immune system and the hypothalamic-pituitary-adrenal (HPA) axis and the immune system which in turn trigger depression.39 In addition to immune stimuli, and physical stress such as infection, chronic inflammation, and tissue injury, exposure to psychological stressors can also induce cytokine expression in the brain.33,36 One of the major environmental factors that may interact with cytokines and genetic predisposition to major depression is stress.31 Physical and psychological stressors can activate immune cells in both the periphery and CNS to release inflammatory cytokines that lead to neurotransmitter changes and behavioral alterations. The immune system is able to detect danger signals by the release of danger associated molecular patterns (DAMPs) through a process known as “sterile inflammation.”DAMPs may serve as a significant bond between stress and inflammatory activity. It is speculated that DAMPs are released during stress. These may generate an immune response through the NLRP3 inflammasome, which is a multiprotein complex involved in the processing of IL-1beta. DAMPs stimulate the inflammasome when lipopolysaccharide (LPS) are present, activating caspase-1, which cleaves the immature precursor of interleukin IL-1beta and IL-18 into their mature releasable forms.This increase in IL-1beta release, allowing the release of other inflammatory cytokines that are released during stress.40
Hippocampus and depression
Cytokines, like IL-6 and TNF-α, are identified as having both neurodegenerative and neuroprotective activities relevant to neuropsychiatric disorders when presented in non-physiological and physiological concentrations, respectively.41 Under stress conditions that induce cytokine production in the brain, the hippocampus (HC) suffers structural changes42,43 that may be associated with the atrophy of the HC in stress-linked depression. Patients with diagnosed MDD show a reduction of hippocampal volume (4-6% smaller) in the left and right HC.44 Evidence of the neurodegenerative activity of IL-6 relies on the association between high IL-6 plasma levels with a reduction in the volume of the HC. However, there is also evidence for the neuroprotective role of this cytokine. High levels of IL-6 are also present when there is an increase of TNF and IL-1β concentrations, suggesting a role of downregulation of neuroinflammation. In addition, healthy subjects that carry the genetic variant rs1800795 of IL-6 show larger volumes on the right side of the hippocampus, which highlights the possible neuroprotective role of IL-6.41 In the other hand, TNF-α may be necessary in brain development and as a modulator of synaptic plasticity when present in low concentrations. Synaptic plasticity is a fundamental mechanism of neuronal adaptation that becomes modified in depression, models of stress in animals and other conditions that alter mood. Increased levels of proinflammatory cytokines, in particular, TNF-α and IL-1 are able to damage synaptic plasticity and cognition promoting the progression of depressive disorders. Patients diagnosed with MDD show large deficits in declarative memory and cognition, mental processes that rely on the ideal functioning of the hippocampus and medial temporal lobe.45
Depression and other illnesses
High rates of depression are usually associated with diseases that involve upregulation of inflammatory processes.37,46,47 Medical illnesses that enhance the appearance of inflammatory markers such as Alzheimer’s disease, MS, obesity, rheumatoid arthritis and gastrointestinal inflammation, promote the development of depression in patients suffering from these diseases at higher rates than in healthy patients.33,40,48 Furthermore, treatments for conditions that include the use of proinflammatory agents such as interferon-gamma (IFN-γ) or IL-2 induce depression. This was proved in patients suffering from chronic infectious hepatitis C and cancer.47,49,50Cancer patients with depression show elevated levels of IL-6 compared to cancer patients without depression.47,51Cardiovascular diseases that are principally caused by atherosclerosis and the associated inflammation of arteries wall can promote the development of depression and vice versa. The use of anti-inflammatory medications (aspirin) to prevent cardiovascular events are associated with the reduction of the symptoms of depression. Exercise also downregulates TNFα and inflammation.52,53 However, healthy patients presenting depression and no comorbidity show elevation of cytokines and its receptors in the CSF, so cytokine levels are not more strongly associated with somatic than psychological symptoms of depression.49,54
Clinical Trials
The NCT00463580 study evaluated the effect of anti-inflammatory monoclonal antibodies in patients with treatment-resistant depression (TRD). It was a single site, parallel-group, randomized, double-blind controlled trial of infliximab versus placebo. Participants were patients with major depression, non-respondent to antidepressant therapies.55 Infliximab is a monoclonal antibody TNF-alpha antagonist that suppresses the body’s response to this cytokine. This study aimed to test the efficacy of infliximab (Remicade®) in reducing symptoms of depression compared to the effects of placebo. High sensitivity c-reactive protein (hs-CRP), TNF-alpha, sTNFRI, andsTNRFII were considered as biomarkers of inflammation and measured at baseline. The results showed that inhibition of TNF-alpha activity could not be regarded as a valid therapeutic strategy for TRD because infliximab did not show improvements in depressive symptoms. However, subjects with an elevated baseline of hs-CRP (hs-CRP>5mg/L) responded better to infliximab, showing a correlation between high inflammation and subsequent response to treatment. Of note, high levels of CRP are due to the increase of Il-6 concentration levels in plasma during inflammation56. Other non-randomised and/or non-placebo trials exhibited improvement of depressive symptoms after treatment with TNF-alpha inhibitors including adalimumab57,58 and etanercept;59 nonetheless, these studies evaluated depressive symptoms comorbid with Crohn’s disease, psoriasis, and psoriasis and psoriatic arthritis, respectively.
Moreover, several clinical trials have demonstrated the neurocognitive processes between proinflammatory cytokines and depression. For this, they used endotoxin, which is a typhoid vaccination that increases cytokine expression, therefore, inducing a depressed mood in healthy patients. For one of the experimentations, neuroimaging was used to evaluate the levels of IL-6 via a whole-brain regression analysis two hours post injection. Results showed that social exclusion leads to depressed mood with a significant difference between males and females, being higher in women.60 Another trial using this same drug evaluated the association of the neural activity with anhedonia (a symptom of depression). Cytokine levels were measured through blood draws every hour to measure plasma levels, and neural activity was recorded using SPM’5. Results showed that there is a significant relationship between inflammatory activity and depressed mood.61
CONCLUSION
Throughout this review, we overviewed the role of cytokines in the immune system, its relationship with serotonin and tryptophan and the conditions that support the inflammatory hypothesis in the physiopathology of depression.Depression is without a doubt a complex disorder and understanding the roles of different processes that contribute to this disorder is a first step to achieve adequate treatment. The importance of this study lies in raising the possibility of finding psychotropic drugs that have a central anti-inflammatory action and that could provide a new generation of antidepressants.
BIBLIOGRAPHY
1. Alberdi J, Taboada O, Castro C, Vázquez C. Depresión. Guías Clínicas. 2006;6:1-6.
2. Sharpley C, Agnew L. Cytokines and depression: findings, issues, and treatment
implications. Rev Neurosci. 2011;22(3):295-302.
implications. Rev Neurosci. 2011;22(3):295-302.
3. Smith R. Cytokines and Depression: How Your Immune System Causes Depression. [Internet]. 1997. [cited 2017 Nov 5] available from: http://www.cytokines-and-depression.com/
4. Köhler O, Benros M, Nordentoft M, Farkouh M, Iyengar R, Mors O, Krogh J. Effect of Anti-inflammatory Treatment on Depression, Depressive Symptoms, and Adverse Effects. JAMA Psychiatry. 2014;71(12):1381-1391.
5. Abbasi S, Hosseini F, Modabbernia A, Ashrafi M, Akhondzadeh S. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: Randomized double-blind placebo-controlled study. J Affect Disord. 2012;141(2-3):308-314.
6. Sowa-Kućma M, Styczeń K, Siwek M, Misztak P, Nowak R, Dudek D, Rybakowski J, Nowak G, Maes M.Lipid Peroxidation and Immune Biomarkers Are Associated with Major Depression and Its Phenotypes, Including Treatment-Resistant Depression and Melancholia. Neurotox Res. 2017.
7. Young J, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord. 2014;169:15-20.
8. Gabbay V, Klein R, Alonso C, Babb J, Nishawala M, De Jesus G. et al. Immune
system dysregulation in adolescent major depressive disorder. J Affect Disord.
2009;115(1-2): 177-182.
system dysregulation in adolescent major depressive disorder. J Affect Disord.
2009;115(1-2): 177-182.
9. Gabbay V, Klein R, Guttman L, Babb J, Alonso C, Nishawala M et al. A Preliminary Study of Cytokines in Suicidal and Nonsuicidal Adolescents with Major Depression. J Child Adolesc Psychopharmacol. 2009;19(4):423-430.
10. Setiawan E, Wilson A, Mizrahi R, Rusjan P, Miller L, Rajkowska G et al. Increased Translocator Protein Distribution Volume, A Marker of Neuroinflammation, in the Brain During Major Depressive Episodes. JAMA Psychiatry. 2015;72(3):268-275.
11. Judd L, Paulus M, Wells K, Rapaport M. Socioeconomic burden of subsyndromal
depressive symptoms and major depression in a sample of the general population.
Am J Psychiatry. 1996;153(11):1411-1417.
depressive symptoms and major depression in a sample of the general population.
Am J Psychiatry. 1996;153(11):1411-1417.
12. Kiecolt-Glaser J, Derry H, Fagundes C. Inflammation: Depression Fans the Flames and Feasts on the Heat. Am J Psychiatry. 2015;172(11):1075-1091.
13. Bai Y, Chiou W, Su T, Li C, Chen M. Pro-inflammatory cytokine associated with
somatic and pain symptoms in depression. J Affect Disord. 2014;155:28-34.
somatic and pain symptoms in depression. J Affect Disord. 2014;155:28-34.
14. Capuron L, Miller A. Immune system to brain signalling: Neuropsychopharmacological implications. Pharmacol Ther. 2011;130(2):226-238.
15. Dantzer R. Cytokine-Induced Sickness Behavior: Where Do We Stand? Brain Behav Immun. 2001;15(1):7-24.
16. Dantzer R, Wollman E, Vitkovic L, Yirmiya R. Cytokines and depression: fortuitous or causative association? Mol Psychiatry. 1999;4(4):328-332.
17. Dunjic-Kostic B, Ivkovic M, Radonjic N, Petronijevic N, Pantovic M, Damjanovic A, Jasovic-Gasic M. Melancholic and atypical major depression — Connection between cytokines, psychopathology and treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2013;43:1-6.
18. Pavón L,Sandoval-López G, Hernández M, Loría F, Estrada I, Pérez M et al. Th2 cytokine response in Major Depressive Disorder patients before treatment. J Neuroimmunol. 2006;172(1-2): 156-165.
19. Raison C, Capuron L, Miller A. Cytokines sing the blues: inflammation and the
pathogenesis of depression. Trends Immunol. 2006;27(1):24-31.
pathogenesis of depression. Trends Immunol. 2006;27(1):24-31.
20. Xie Z, Wang X, Xu N, Wang J, Pan W, Tang X, Yang J. Alterations in the inflammatory cytokines and brain-derived neurotrophic factor contribute to depression-like phenotype after spared nerve injury: improvement by ketamine. Sci Rep. 2017;7(1):3124.
21. Obrien S, Scott L, Dinan T. Cytokines: abnormalities in major depression and
implications for pharmacological treatment. Hum Psychopharmacol. 2004;19(6):397-403.
implications for pharmacological treatment. Hum Psychopharmacol. 2004;19(6):397-403.
22. Dinarello C. Interleukin-1. Cytokine Growth Factor Rev. 1997;8(4):253-265.
23. Chu W. Tumor necrosis factor. Cancer Lett. 2012;328(2):222-225.
24. Feltes P, Doorduin J, Klein H., Juárez-Orozco L, Dierckx R, Moriguchi-Jeckel C,
de Vries E. Anti-inflammatory treatment for major depressive disorder:
implications for patients with an elevated immune profile and non-responders to
standard antidepressant therapy. J Psychopharmacol. 2017;31(9):1149-1165.
de Vries E. Anti-inflammatory treatment for major depressive disorder:
implications for patients with an elevated immune profile and non-responders to
standard antidepressant therapy. J Psychopharmacol. 2017;31(9):1149-1165.
25. Simpson R, Hammercher A, Smith D, Mathews J, Ward L. Interleukin-6: Structure-function relationships. Protein Sci. 1997;6(5):929-955.
26. Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther. 2006;8(Suppl 2):S3.
27. Hannon J, Hoyer D. Molecular biology of 5-HT receptors. Behav Brain Res.
2008;195(1): 198-213.
2008;195(1): 198-213.
28. Dantzer R, O’Connor J, Lawson M,Kelley K. Inflammation-associated depression: From serotonin to kynurenine. Psychoneuroendocrinology. 2011;36(3):426-436.
29. Zhu C, Blakely R, Hewlett W. The Proinflammatory Cytokines Interleukin-1beta and Tumor Necrosis Factor-Alpha Activate Serotonin Transporters.
Neuropsychopharmacology. 2006;31(10):2121-2131.
Neuropsychopharmacology. 2006;31(10):2121-2131.
30. Baranyi A, Amouzadeh-Ghadikolai O, von Lewinski D, Breitenecker R, Rothenhäusler H, Robier C et al. Revisting the tryptophan-resotonin deficiency and the inflammatory hypotheses of major depression in a biopsychosocial approach. Peerj. 5:e3968
31. Haroon E, Raison C, Miller A. Psychoneuroimmunology Meets Neuropsychopharmacology: Translational Implications of the Impact of Inflammation on Behavior. Neuropsychopharmacology. 2012;37(1):137-162.
32. Lichtblau N, Schmidt F, Schumann R, Kirkby K, Himmerich H. Cytokines as biomarkers in depressive disorder: Current standing and prospects. Int Rev Psychiatry. 2013;25(5):592-603.
33. Schiepers O, Wichers M, Maes M. Cytokines and major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29(2):201-217.
34. Shelton R, Claiborne J, Sidoryk-Wegrzynowicz M, Reddy R, Aschner M, Lewis D, Mirnics K. Altered expression of genes involved in inflammation and apoptosis in frontal cortex in major depression. Mol Psychiatry. 2011;16(7):751-762.
35. Loftis J, Huckans M, Morasco B. Neuroimmune mechanisms of cytokine-induced depression: Current theories and novel treatment strategies. Neurobiol Dis. 2010;37(3):519-533.
36. Capuron L, Dantzer R. Cytokines and depression: The need for a new paradigm. Brain Behav Immun. 2003;17 (Suppl 1):S119-124.
37. Dantzer R, O’ Connor J, Freund G, Johnson R, Kelley K. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008; 9(1): 46-56.
38. Iwata M, Ota K, Duman R. The inflammasome: Pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun. 2013;31:105-114.
39. Leonard B. The Concept of Depression as a Dysfunction of the Immune System. Curr Immunol Rev. 2010;6(3): 205-212.
40. Felger J, Lotrich F. Inflammatory cytokines in depression: Neurobiological mechanisms and therapeutic implications.Neuroscience. 2013;246:199-229.
41. Baune B, Konrad C, Grotegerd D, Suslow T, Birosova E, Ohrmann P et al. Interleukin-6 gene (IL-6): a possible role in brain morphology in the healthy adult brain. J Neuroinflammation. 2012;9:125.
42. Malberg J, Duman R. Cell Proliferation in Adult Hippocampus is Decreased by Inescapable Stress: Reversal by Fluoxetine Treatment. Neuropsychopharmacology. 2003;28(9):1562-1571.
43. Miller A, Raison C. Are Anti-inflammatory Therapies Viable Treatments for Psychiatric Disorders? Where the Rubber Meets the Road. JAMA Psychiatry. 2015;72(6):527-528.
44. Campbell S, Marriott M, Nahmias C, MacQueen G. Lower Hippocampal Volume in Patients Suffering From Depression: A Meta-Analysis. Am J Psychiatry.
2004;161(4):598-607.
2004;161(4):598-607.
45. Khairova R, Machado-Vieira R, Du J, Manji H. A potential role for pro-inflammatory cytokines in regulating synaptic plasticity in major depressive disorder. Int J Neuropsychopharmacol. 2009;12(4):561-578.
46. Farooq R, Asghar K, Kanwal S, Zulqernain A. Role of inflammatory cytokines in
depression: Focus on interleukin-1β. Biomed Rep. 2017;6(1):15-20.
depression: Focus on interleukin-1β. Biomed Rep. 2017;6(1):15-20.
47. O’Connor M, Irwin M, Sheldon J, Kwan L, Ganz P. Pro-inflammatory cytokines and depression in a familial cancer registry. Psychooncology. 2007;16(5):499-501.
48. Yirmiya R, Pollak Y, Morag M, Reichenberg A, Barak O, Avitsur R, Pollmächer T. Illness, Cytokines and Depression. Ann N Y Acad Sci. 2000;917:478-487.
49. Miller A, Maletic V, Raison C. Inflammation and Its Discontents: The Role of Cytokines in the Pathophysiology of Major Depression. Biol Psychiatry. 2009;65(9):732-741.
50. Pasic J, Levy W, Sullivan M. Cytokines in Depression and Heart Failure. Psychosom Med. 2003;65(2):181-193.
51. Breitbart W, Rosenfeld B, Tobias K, Pessin H, Ku G. Y, Yuan J, Wolchok J.
Depression, cytokines, and pancreatic cancer. Psychooncology. 2014;23(3):339-345.
Depression, cytokines, and pancreatic cancer. Psychooncology. 2014;23(3):339-345.
52. Funk J, Gohlke J, Kraft A, McPherson C, Collins J, Jean Harry G. Voluntary exercise protects hippocampal neurons from trimethyltin injury: Possible role of
interleukin-6 to modulate tumor necrosis factor receptor-mediated neurotoxicity. Brain Behav Immun. 2011;25(6):1063-1077.
interleukin-6 to modulate tumor necrosis factor receptor-mediated neurotoxicity. Brain Behav Immun. 2011;25(6):1063-1077.
53. Hiles S, Baker A, Malmanche T, Mcevoy M, Boyle M, Attia J. The role of inflammatory markers in explaining the association between depression and cardiovascular hospitalisations. J Behav Med. 2015;38(4):609-619.
54. Einvik G, Vistnes M, Hrubos-Strøm H, Randby A, Namtvedt S, Nordhus I et al.
Circulating cytokine concentrations are not associated with major depressive
disorder in a community-based cohort. Gen Hosp Psychiatry. 2012;34(3):262-267.
Circulating cytokine concentrations are not associated with major depressive
disorder in a community-based cohort. Gen Hosp Psychiatry. 2012;34(3):262-267.
55. Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF et al. A
randomized controlled trial of the tumor necrosis factor antagonist infliximab
for treatment-resistant depression: the role of baseline inflammatory
biomarkers. JAMA Psychiatry 2013;70(1):31–41.
randomized controlled trial of the tumor necrosis factor antagonist infliximab
for treatment-resistant depression: the role of baseline inflammatory
biomarkers. JAMA Psychiatry 2013;70(1):31–41.
56. Seo HS. The Role and Clinical Significance of High-Sensitivity C-Reactive Protein in Cardiovascular Disease. Korean Circ J. 2012;42(3):151-153.
57. Loftus EV, Feagan BG, Colombel JF, Rubin DT, Wu EQ, Yu AP et al. Effects of adalimumab maintenance therapy on health-related quality of life of patients with Crohn’s disease: patient-reported outcomes of the CHARM trial. Am J Gastroenterol 2008;103(12): 3132–3141.
58. Guh D, Papp K, Lynde C, Bansback N, Zhang W, Qian H et al. Impact of adalimumab on quality of life and depression in psoriasis patients: results from PRIDE. Value Health 2010; 132010: A148.
59. Gniadecki R, Robertson D, Molta CT, Freundlich B, Pedersen R, Li W et al. Self-reported health outcomes in patients with psoriasis and psoriatic arthritis randomized to two etanercept regimens. J Eur Acad Dermatol Venereol. 2012;26(11):1436–1443.
60. Eisenberger NI, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. An fMRI study of cytokine-induced depressed mood and social pain: The role of sex differences. NeuroImage. 2009;47(3):881–90.
61. Eisenberger NI, Berkman ET, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. Inflammation-Induced Anhedonia: Endotoxin Reduces Ventral Striatum Responses to Reward. Biological Psychiatry. 2010;68(8):748–54.
Received: 20 December 2017
Approved: 2 February 2018
María Belén Paredes, María Eugenia Sulen
Yachay Tech University, Ciudad del Conocimiento Yachay, Urcuquí, Imbabura, Ecuador 100119
maria.paredes@yachaytech.edu.ec, maria.sulen@yachaytech.edu.ec



















